Table of Contents
Congenital Heart Defect
Also known as congenital heart disease, congenital heart defect (CHD) is a deformation occurred during embryonic life; that is, a malformation of the heart present at birth. It is a very common heart condition affecting approximately 7 to 8 births out of 1000. Heart defects s responsible for about 6% of pediatric hospitalizations.
Although congenital heart defect is a serious disease, a vast majority of patients recover without a medical treatment. Even when the disease requires medical treatment (taking medication or surgical intervention), it often has an excellent prognosis; in fact, most heart defect cases that need medical intervention are treated without complications. Unfortunately, some children die of CHD.
Congenital heart disease is divided into two main types; each one of them has many subtypes (see causes for subtypes).
Cyanotic heart defect – this type of heart defect is also called “blue disease” because of the bluish-tint color takes the skin of children suffering from the defect. The discoloration of the skin is due to a short circuit (shunt) that connects directly the oxygen-poor blood, from the vena cava, with blood rich in oxygen flowing to the aorta. The defect causes the positions of the aorta and pulmonary artery to reverse, thus, preventing the blood to pass through the lungs where it picks up oxygen.
 Acyanotic heart defect– acyanotic heart disease is, most often, caused by a narrowing of blood vessels or an abnormal communication between the heart chambers. In other words, when your child has acyanotic heart defect, he has a decreased blood flow in his lower body due to a narrowing of the aorta, the artery that delivers oxygenated blood to all parts of body. Sometimes, the obstruction can be localized in the pulmonary artery, the artery that carries non-oxygenated blood from the heart to the lungs.
Acyanotic heart defect– acyanotic heart disease is, most often, caused by a narrowing of blood vessels or an abnormal communication between the heart chambers. In other words, when your child has acyanotic heart defect, he has a decreased blood flow in his lower body due to a narrowing of the aorta, the artery that delivers oxygenated blood to all parts of body. Sometimes, the obstruction can be localized in the pulmonary artery, the artery that carries non-oxygenated blood from the heart to the lungs.
In some cases, however, the defect is due to the lack of closure of a small cardiac canal presents in the fetus, causing the blood to pass directly from the aorta to the pulmonary artery. Similarly, an opening may be abnormally present in the lining of the heart, thus creating a communication between the two ventricles or the two atria.
Congenital Heart Defect Causes and Risk Factors
Scientists believe that many causes can lead to heart defects. In general, congenital heart defects exist when there is a:
- Abnormal interventricular communication – communication between a ventricle and an atrium causing direct passage of blood from the aorta to the pulmonary artery, this condition is a subtype of acyanotic heart defect.
- Atrial septal defect (ASD) – this form of heart defect is characterized by the presence of a pathological hole between the two upper chambers of the heart causing communication between the atria. atrial septal defect is a subtype of acyanotic heart defect.
- Coarctation of the aorta – this medical term refers to narrowing of the thoracic aorta. The aorta allows distribution of oxygenated blood from the left ventricle to the whole body; when, due to certain circumstance it becomes narrowed, there is a decreased blood flow in the lower body. Coarctation of the aorta is a subtype of acyanotic heart defect.
- Aortic stenosis – also called aortic valve stenosis, this form of heart defect is due to a narrowing of a portion of the aorta between the aortic valves; the condition leads to a restriction of blood flow from the left ventricle and the aorta during contraction of the heart chambers (systole). Aortic valve stenosis may be present from birth (congenital), or it may develop later in life (acquired).
- Pulmonary valve stenosis – also known as valvular pulmonary stenosis (PS), pulmonary valve stenosis is medical condition characterized by narrowing of the pulmonary artery – the artery that carries non-oxygenated blood from the heart to the lungs. Its narrowing cause the heart to be unable to receive adequate oxygenated blood needed to function properly. Pulmonary valve stenosis is a subtype of acyanotic heart defect.
- transposition of the great vessels (TGV) – also known as ventriculo-arterial discordance, the TGV is a congenital heart defect very common in newborns; it is responsible for cyanosis, the blue color that take the skin and mucous membranes when blood contains more than 5% of reduced hemoglobin. Transposition of the great vessels is a subtype of cyanotic heart defect.
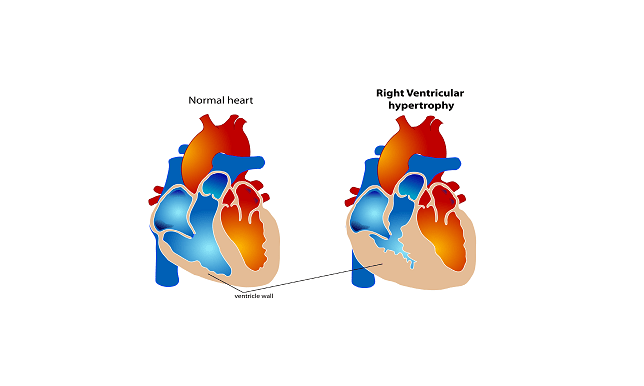
- Tetralogy of Fallot (TOF) – this condition is the most common form of cyanotic congenital heart disease, representing nearly 8% of all congenital heart defects. Tetra means four. That is, TOF is a combination of four defects: pulmonary stenosis, ventricular septal defect, right ventricular hypertrophy and malposition of the aorta (also called overriding aorta). Tetralogy of Fallot is subtype of cyanotic congenital heart defect.
- Trilogy of Fallot – “tri”menas three. That is, Trilogy of Fallot is a congenital heart defect associated with three abnormalities: pulmonary valve stenosis, right ventricular hypertrophy and atrial septal defect. Trilogy of Fallot is subtype of cyanotic congenital heart defect.
Congenital heart defects occur during the formation of the heart during intrauterine life. That is, the lifestyle of the mother can plays a major role in the development of the defect in the fetus. However, the causes of the disease are not well known; some factors, however, appear to play a role in its occurrence.
- Rubella (German measles) – suffering from rubella while you are pregnant increases the risk of your infant to develop congenital heart disease
- Diabetes – besides gestational diabetes, having diabetes 1 or 2 may affect your fetus’ heart development and functioning.
- Heredity – approximately 5% of heart defects are related to genetic. Certain chromosomal diseases such as trisomy 21 are associated with an increased risk of heart problems. Congenital heart disease tend to run in families
- Drug intoxication – Heavy alcohol consumption during pregnancy and intoxication with certain medications such as isotretinoin (Accutane) and lithium (Eskalith, Lithobid) can cause heart problems in your fetus including congenital heart defects.
Congenital Heart Defect Symptoms
Symptoms of congenital heart defects vary depending on the nature and severity of the disease. In addition, most heart defects do not always manifest at the beginning; some patients may experience symptoms a few years after birth or even during adulthood.
In general, if you or your child has a heart defect, at least one of the following symptoms will develop:
- growth Disorders
- dizziness
- fainting
- unreasonable discomfort
- abnormal heart rhythms (arrhythmias)
- shortness of breath or difficulty breathing (dyspnea)
- swelling of body tissue or organs (edema)
- blue coloration of the skin and mucous membranes (cyanosis)
- Elevated temperature, which may explain infection of the endocardium.
Complications
In most cases, congenital heart defects do not cause complications. However, some types of cyanotic heart disease, especially tetralogy of Fallot can be life threatening, mainly in children. The most common complication of congenital heart defect is endocarditis, infection of cells lining the inside of the heart (endocardium). In addition, heart defects can lead to development of:
- Stroke
- Heart failure
- Heart valve problems
- Pulmonary hypertension.
Diagnosis

The first step in heart defect diagnosis is a physical examination. Your cardiologist will search for signs of the disease, and ask you appropriate questions which can indicate the pathology. In addition, your doctor may check your child medical history looking for disorders that can lead to cardiomyopathy. To diagnose a heart defect, several tests are necessary to establish an accurate diagnosis:
Chest x-ray – this exam is performed to create picture of the heart muscle, lungs and bones forming the thoracic cage. It allows your doctor to detect abnormality in your child’s heart shape and size. In addition, it confirms the presence of a valve disorder and provides important details about the problem and severity.
Electrocardiogram (ECG) – This test allows your cardiologist to study the functioning of the heart by measuring its electrical activity. Each heart beat produces an electrical signal that spreads from the top of the heart to the bottom. This signal causes the heart to contract and pump blood throughout the body. Using these electrical signals, your health care provider can determine the pace of heartbeats, if the heart is dilated or overworking.
By measuring the time it takes the electrical impulse to travel through the heart, your cardiologist can determine if electrical activity is normal, fast or irregular.
Cardiac ultrasound (Echocardiogram) – an echocardiogram is ultrasound test that your health care provider can use to create picture moving picture of the heart. It consists of using sound waves. The waves recorded to helps determine the shape, texture and movement of the valves and the volume and function of cardiac chambers. A cardiac ultrasound can also be used to detect blood clots inside the heart.
Cardiac catheterization (heart cath) – to determine the severity of the defect and its effect on your heart, your cardiologist can recommend a heart cath. During the procedure, he will insert a thin catheter in an artery or vein, and pass it through your blood vessel to your heart chamber to perform certain therapeutic or diagnostic procedures: angioplasty, angiography, balloon septostomy, electrophysiology study, etc.
In addition, a cardiac catheterization allows your health care provider to measure your blood oxygen saturation level, and detect reflux of blood from the aorta to the left ventricle.
Cardiac stress test – your cardiologist can recommend a stress test (or exercise test) to measure your heart’s performance both at rest and while in activity.
Congenital Heart Defect Treatment
A child with heart defect, although should be treated as all other children, must be limited to intense exercise. Therefore, it is important to talk to your doctor before you leave him/her make some efforts or walking a long journey.
Congenital heart defect treatment is medico-surgical. The treatment can be designed to treat the disease itself or the problems related to it. Heart defect treatment can be medication, surgery or both. Medication taken or surgery performed depends on type of defect and its severity. Some congenital heart diseases such as pulmonary valve stenosis, ductus arteriosus, and atrial septal defect require surgical treatment. In most cases, surgery allows the child to adopt a normal life.
Medications – in the case the heart defect does not pose a great risk of death, your doctor may use appropriate diuretics to help the heart work more efficiently. In addition, your child may be prescribed an antibiotherapy if the disease is associated with myocarditis, inflammation of the heart muscle due to viral infection. Antibiotics should be taken non-stopped as recommended. If for any reason your child cannot continue the treatment, consult your physician before taking any decision.
Catheterization technique – this is a surgical technique usually performed under local anesthesia. During the procedure, an interventional cardiologist inserts a catheter into a leg, groin, neck or arm vein of your child and guides it to the heart using a radiographic apparatus. This technique allows not only to seeing the defect but also repairing it.
Surgical treatment
Open-heart surgery – if all non surgical treatments do not work, surgery is the ideal choice to treat a congenital heart defect; in fact, surgical intervention often performed to treat most heart defects. The intervention aims to restore normal cardiac physiology. During the procedure, an incision is made vertically in the middle of the breastbone to gain full access to the heart and fix the defect. In general, after the intervention, the child remains a few days in an intensive care unit. After hospitalization, rehabilitation is important to teach the child/infant the following:
- respiratory movements
- lifting
- walking
- gymnastics
- retraining of the heart during exercise…
Cardiac transplantation – a heart transplant is an advanced surgical procedure performed to replace a diseased heart with a healthy one, usually taken from a donor. Heart transplant should be the last step in the treatment of heart defect; it should be performed after all other options are not effective. En general, your cardio surgeon will recommend heart transplantation in cases of severe and irreversible heart failure, for which life expectancy is limited. Complications related to a cardiac transplantation include:
- Infectious complications following the surgery
- graft rejection by the recipient’s immune system, which requires immunosuppressive therapy.
- occurrence of cancer due to immunosuppressive action of the drugs in your body.
Congenital Heart Defect Prevention
There is no specific method to prevent heart defect; however, if you are pregnant or planning to become pregnant, it is important to live a healthy lifestyle. Excising regularly, losing weight (if you are obese or overweight) and stopping smoking (including second hand smoke) are the best ways to prevent all major cardiovascular disease. In addition, you need to consume a healthy diet.
- Increase your intake of antioxidants
- Avoid saturated acids, mainly from animal fats, pastries, margarine, etc.
- Increase your intake of carbohydrates and fiber; they play an important role in increasing the levels of good cholesterol
- Reduce bad cholesterol: egg yolk, organ meats (brain, kidney, liver), nuts, almonds, lobster, shellfish, fish eggs, etc.
- Eat polyunsaturated fatty acids such as omega-6 (sunflower oil) omega 3 (flax seed oil, fish oil); they lower the bad LDL cholesterol and prevent the formation of a blood clot.
- Eat plenty of fruits (2 to 3 per day), vegetables (3 to 4 servings per day), polyphenols (moderate consumption of wine and green tea) and phyto-oestrogens: soy, green tea, chickpeas, lentils, beans, grains, carrots, fennel, onions, garlic, etc.
References:
1 – http://www.nlm.nih.gov/medlineplus/ency/article/000157.htm
2 – Hoffman JI, Kaplan S (June 2002). “The incidence of congenital heart disease”. J. Am. Coll. Cardiol. 39 (12): 1890–900. doi:10.1016/S0735-1097(02)01886-7. PMID 12084585.
3 – “What Are Congenital Heart Defects?”. National Heart, Lung, and Blood Institute. July 1, 2011. Retrieved 10 August 2015.
4 – Shanthi Mendis; Pekka Puska; Bo Norrving; World Health Organization (2011). Global Atlas on Cardiovascular Disease Prevention and Control (PDF). World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization. pp. 3, 60. ISBN 978-92-4-156437-3.
5 – Tidyman, W. E.; Rauen, K. A. (2009). “The RASopathies: developmental syndromes of Ras/MAPK pathway dysregulation”. Current Opinion in Genetics & Development 19 (3): 230–6. doi:10.1016/j.gde.2009.04.001. PMC 2743116. PMID 19467855.
6 – “Factors Contributing to Congenital Heart Disease”. Lucile Packard Children’s Hospital at Stanford. Retrieved 30 July 2010.
7 – Mills JL, Troendle J, Conley MR, Carter T, Druschel CM (June 2010). “Maternal obesity and congenital heart defects: a population-based study”. Am. J. Clin. Nutr. 91 (6): 1543–9. doi:10.3945/ajcn.2009.28865. PMC 2869507. PMID 20375192.
8 – Rasmussen SA, Galuska DA (June 2010). “Prepregnancy obesity and birth defects: what’s next?”. Am. J. Clin. Nutr. 91 (6): 1539–40. doi:10.3945/ajcn.2010.29666. PMID 20427732.
9 – Larsen, William J. (1993). “7. Development of the Heart”. Human Embryology. Churchill Livingstone. ISBN 0-443-08724-5.
10 – MedlinePlus Encyclopedia Fetal echocardiography
11 – http://www.nhs.uk/Conditions/Congenital-heart-disease/Pages/Diagnosis.aspx
12 – Thomas P. Shanley; Derek S. Wheeler; Hector R. Wong (2007). Pediatric critical care medicine: basic science and clinical evidence. Berlin: Springer. p. 666. ISBN 1-84628-463-5.
13 – “Hypoplastic Left Heart Syndrome”. American Heart. Retrieved 30 July 2010.