Table of Contents
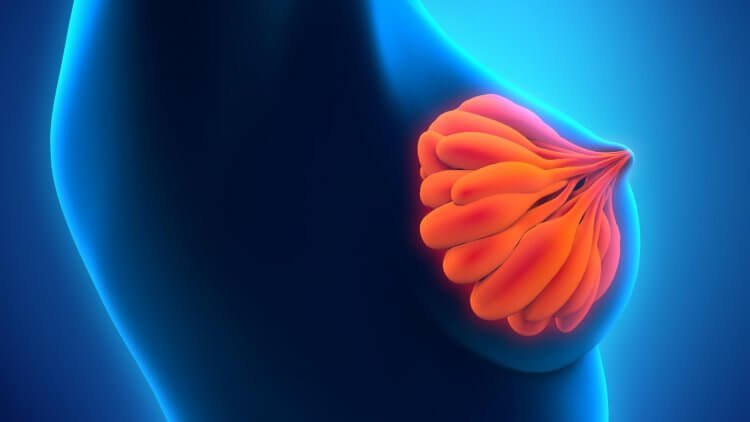
Mastitis, a common condition affecting lactating women, involves inflammation of the breast tissue. It can cause discomfort and hinder breastfeeding. While it often occurs during the early stages of breastfeeding, mastitis can also develop at any point during lactation. Understanding the causes, symptoms, treatment options, and preventive measures is crucial for managing this condition effectively.
Mastitis occurs when the breast tissue becomes inflamed, resulting in pain, redness, and swelling. It is most often caused by a combination of factors such as hormonal fluctuations, blocked milk ducts, and bacterial infection. Though it can be distressing, timely and appropriate treatment can help alleviate the symptoms and prevent complications. It is not breast cancer.
Causes of Mastitis
Mastitis is usually caused by an infection. Several factors can contribute to the development of mastitis:
Hormonal Fluctuations – Hormones play a significant role in lactation, and fluctuations in hormone levels can impact milk production and flow. During the early stages of breastfeeding, hormonal changes trigger the body to produce and release milk. However, if there’s an imbalance in these hormones, it can lead to poor drainage of milk from the breasts, increasing the risk of inflammation and infection. Additionally, abrupt weaning or irregular breastfeeding patterns can disrupt hormone regulation, further contributing to mastitis development.
Blocked Milk Ducts – Blocked milk ducts are a common precursor to mastitis. When milk is not adequately removed from the breasts, it can accumulate and create pressure within the ducts. This blockage restricts milk flow and sets the stage for inflammation. A variety of factors can lead to blocked ducts, including improper latch technique, infrequent breastfeeding or pumping, wearing tight clothing that compresses the breasts, or even pressure on the breasts from sleeping in an uncomfortable position.
Bacterial Infection – Bacterial infection is another key factor in mastitis. Bacteria, often from the baby’s mouth or the mother’s skin, can enter the breast through cracked or damaged nipples. This can lead to an infection in the breast tissue. Staphylococcus aureus is a common bacterium that can enter the breast tissue, leading to localized infection and inflammation. The infection triggers the body’s immune response, resulting in swelling, redness, and the characteristic symptoms of mastitis.
Other factors suspected in causing mastitis include:
Incomplete Emptying of the Breast: When the breast is not adequately emptied during breastfeeding, milk can build up in the milk ducts, leading to a higher risk of infection.
Engorgement: Engorgement occurs when the breasts become overly full with milk, causing pressure and constriction of milk ducts. This can create an environment conducive to infection.
Poor Latching: If a baby doesn’t latch onto the breast properly, it can lead to inefficient milk removal and subsequent milk stasis, increasing the risk of mastitis.
Breast Trauma: Any trauma to the breast, such as a blow or injury, can disrupt the breast tissue and potentially lead to infection.
Weakened Immune System: A weakened immune system can make an individual more susceptible to infections, including mastitis.
Nipple Damage: Cracked or damaged nipples can provide an entry point for bacteria, increasing the risk of infection.
Stress and Fatigue: High levels of stress and fatigue can compromise the body’s ability to fight off infections, making a person more vulnerable to mastitis.
Infrequent or Irregular Feeding: Not breastfeeding regularly or on a consistent schedule can lead to milk accumulation and increased susceptibility to infection.
Breast Surgery: Any previous breast surgery, such as augmentation or reduction, can alter breast tissue and ducts, potentially increasing the likelihood of mastitis.
Use of Tight-Fitting Bras: Wearing bras that are too tight or constricting can impede proper milk flow and contribute to the development of mastitis.
Poor Breast Hygiene: Inadequate breast hygiene, such as not cleaning the nipples properly before breastfeeding, can introduce bacteria and increase infection risk.
Mastitis Symptoms
Recognizing the early signs and symptoms of mastitis is crucial for prompt intervention and effective management. This section explores the common mastitis symptoms, shedding light on the indicators that can help individuals identify and address this condition in its early stages. Understanding these symptoms empowers you to take proactive steps towards seeking appropriate medical care and maintaining their overall breast health.
The following are common mastitis symptoms:
Breast Pain and Swelling – Breast pain and swelling are hallmark symptoms of mastitis. The affected breast may feel tender to the touch and appear visibly enlarged. The pain can range from a dull ache to a throbbing sensation, and it’s often exacerbated when pressure is applied or during breastfeeding.
Redness and Warmth – Inflammation caused by mastitis can lead to noticeable redness and warmth in the affected breast. The skin may appear redder than usual, and the breast itself might feel warm to the touch. This localized redness is a clear indicator of the inflammatory response taking place.
Flu-like Symptoms – Mastitis can cause flu-like symptoms, which can be particularly surprising to those experiencing it. Fever, chills, and fatigue are common systemic responses to infection and inflammation. The immune system’s activation in response to the infection leads to these symptoms, often causing individuals to feel unwell and fatigued.
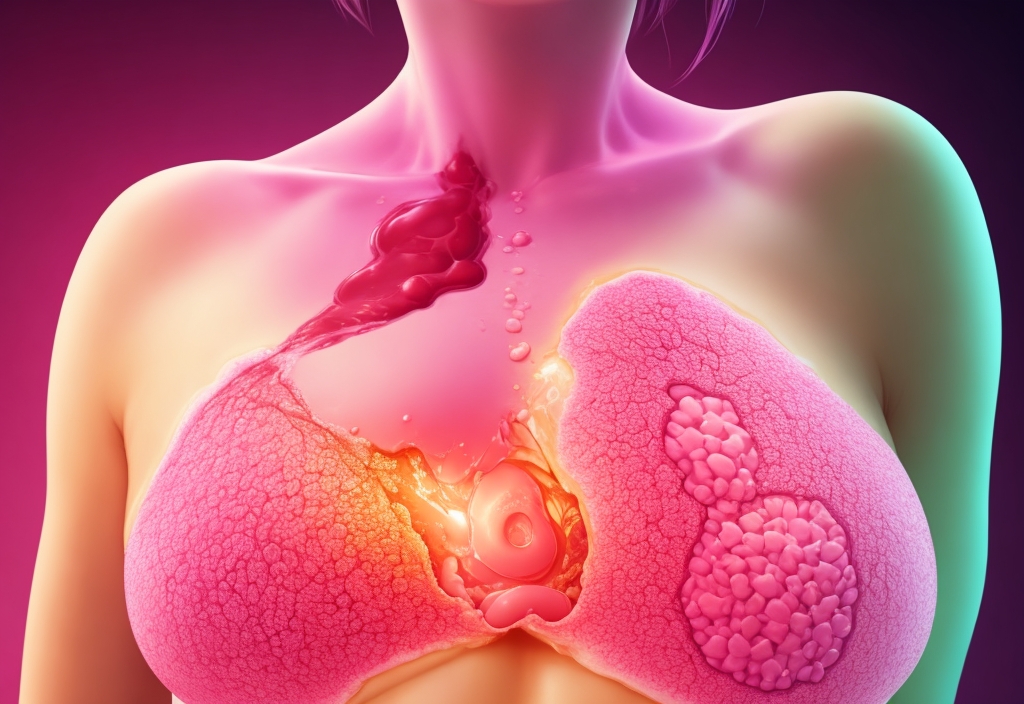
Abscess Formation (Advanced Cases) – In more severe cases of mastitis, especially if left untreated, an abscess can form within the breast tissue. An abscess is a collection of pus that results from the body’s attempt to contain and fight the infection. Abscesses typically present as a painful lump within the breast, accompanied by significant discomfort and swelling.
Breast Engorgement: The affected breast might become engorged and feel unusually full, with increased pressure and tightness. This can be a result of inadequate milk drainage.
Nipple Discharge: In some cases, pus or other discharge may be observed from the nipple. This indicates the presence of infection within the breast tissue.
General Malaise: Individuals with mastitis often experience a sense of fatigue, overall discomfort, and a decrease in energy levels.
Nipple Cracking or Damage: If the nipple is cracked, damaged, or experiencing trauma, it can create an entry point for bacteria, potentially leading to mastitis.
Unilateral Symptoms: Mastitis typically affects one breast, leading to symptoms localized to that side of the body.
Understanding the causes and symptoms of mastitis is crucial for timely intervention and effective management. If you suspect you have mastitis or are experiencing any of these symptoms, seeking medical advice is important to ensure proper treatment and prevent complications.
Mastitis Treatment Options
When mastitis is suspected or diagnosed, timely and appropriate treatment is essential to alleviate symptoms, address the infection, and prevent complications. The following are common treatment options for mastitis:
Continued Breastfeeding or Pumping: Contrary to what might be assumed, continuing to breastfeed from the affected breast is often recommended during mastitis. Frequent and effective breastfeeding helps ensure that the breast is adequately emptied, reducing milk accumulation and preventing further inflammation. Emptying the breast also helps clear any blocked milk ducts, promoting healing and relieving symptoms.
Frequent Milk Removal: Breastfeed or pump more frequently than usual to ensure the breast is adequately emptied, reducing milk buildup and improving symptoms.
Warm Compresses: Applying warm compresses to the affected breast before breastfeeding or pumping can help alleviate pain, promote milk flow, and reduce inflammation.
Massage: Gently massaging the affected breast while breastfeeding or pumping can help break up any milk clots and improve milk flow.
Pain Relief: Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can offer relief from the discomfort associated with mastitis. These medications help reduce inflammation and alleviate breast pain. Applying warm compresses to the affected breast before breastfeeding can also aid in pain relief and encourage milk flow, making the breastfeeding process more comfortable.
Rest and Hydration: Getting adequate rest and staying hydrated support the body’s natural healing processes.
Antibiotics: If the mastitis is caused by a bacterial infection, healthcare professionals might prescribe antibiotics. Completing the full course of antibiotics is crucial to effectively clear the infection.
Consulting a Healthcare Provider: If symptoms persist or worsen despite home remedies, consult a healthcare provider. They can provide a proper diagnosis, adjust treatment, and ensure that the infection is properly managed.
Adjusting Breastfeeding Technique: A lactation consultant can help assess and improve breastfeeding techniques to prevent recurrence and promote better milk drainage.
Cold Compresses: After breastfeeding or pumping, applying cold compresses can help reduce swelling and provide relief.
Abscess Drainage: In severe cases where an abscess (pus-filled pocket) forms, drainage may be necessary. This procedure is usually performed by a medical professional.
Supportive Measures: Supportive bras that fit properly and don’t constrict the breasts can help prevent further discomfort.
Avoiding Tight Clothing: Wear loose clothing that doesn’t put pressure on the breasts, allowing better circulation and reducing inflammation.
It’s crucial to work closely with a healthcare provider, especially if symptoms are severe, there is no improvement with treatment, or there are signs of an abscess. Prompt and appropriate treatment can help resolve mastitis efficiently, preventing complications and ensuring a smoother recovery.
Mastitis Alternative Treatments
Managing mastitis requires a comprehensive approach that addresses both the physical symptoms and the underlying causes. By combining medical interventions, pain relief strategies, and dietary considerations, individuals can navigate mastitis more comfortably and facilitate a smoother recovery. If symptoms persist or worsen despite treatment efforts, seeking medical attention is recommended to prevent potential complications.
Hydration and Nutrition – Staying hydrated and maintaining a balanced diet are crucial for overall health and optimal lactation. Drinking enough water ensures that the body can produce an adequate milk supply and support the healing process. Consuming nutrient-rich foods, including fruits, vegetables, whole grains, and lean proteins, provides the body with the energy and nutrients it needs to recover.
Herbal Supplements – While scientific research on the effectiveness of herbal supplements in treating mastitis is limited, some individuals find relief from certain remedies. Lecithin supplements, for example, are believed to reduce the viscosity of breast milk and prevent blockages. Probiotics might help maintain a healthy balance of bacteria within the body. However, it’s essential to consult with a healthcare professional before introducing any herbal supplements, especially if you’re already on prescribed medications.
Avoiding Irritants – Certain foods and beverages can potentially exacerbate inflammation and discomfort. For some individuals, caffeine, spicy foods, and even certain dairy products might contribute to breast discomfort. Temporarily avoiding these irritants during the course of mastitis can help alleviate symptoms and promote healing.
Mastitis Prevention
Preventing mastitis is not only about avoiding pain and discomfort; it also contributes to the continuation of successful breastfeeding. Prioritizing mastitis prevention is a proactive approach to maintaining breast health and ensuring a positive breastfeeding experience. By adopting proper breastfeeding techniques, maintaining hygiene, staying hydrated, managing stress, and avoiding unnecessary pressure on your breasts, you can significantly reduce the risk of mastitis and focus on enjoying the precious moments of motherhood.
Ensuring a Correct Latch – A proper latch is crucial for effective breastfeeding. When your baby latches correctly, they can drain your breasts adequately, reducing the likelihood of blocked milk ducts.
Frequent Feeding or Pumping – Frequent feeding or pumping helps in maintaining milk flow and preventing engorgement. Ensuring that your breasts are emptied regularly can reduce the risk of milk buildup and subsequent inflammation.
Clean Hands and Nipple Care – Practicing good hygiene is essential to prevent infection. Wash your hands before touching your breasts or your baby, and keep your nipples clean. Avoid using harsh soaps on your nipples, as they can strip away natural oils.
Avoid Tight Clothing – Wearing tight-fitting bras or clothing can put pressure on your breasts, potentially leading to blocked ducts. Opt for well-fitting, breathable clothing to prevent unnecessary discomfort.
Staying Hydrated and Well-Nourished – Hydration Impacts your breasts’ health. Staying hydrated supports milk production and overall breast health. Drink plenty of water throughout the day to maintain optimal milk supply.
Nutrient-Rich Diet – Eating a balanced and nutrient-rich diet provides your body with the energy it needs for breastfeeding. Incorporate foods rich in vitamins, minerals, and antioxidants to support your immune system.
Managing Stress – Stress can have a negative impact on your body, including your breast health. Practicing relaxation techniques, such as deep breathing, meditation, or gentle exercises, can help reduce stress levels and promote breast health.
Avoiding Unnecessary Pressure – Proper baby carrier use is also important. When using a baby carrier, ensure that it doesn’t put pressure on your breasts. Improper positioning can lead to blocked ducts and discomfort.
Sleeping Position – Choose a comfortable sleeping position that doesn’t compress your breasts. If you’re a side sleeper, consider using pillows for support and to prevent unnecessary pressure on your breasts.
Mastitis Herbal Remedies
Cabbage Leaves (Europe) – In various European cultures, cabbage leaves have been used as a natural remedy for mastitis. Chilled cabbage leaves can provide relief by reducing inflammation and discomfort. Applying cabbage leaves to the breasts can also help draw out excess fluid and promote healing. While scientific evidence is limited, some individuals find this remedy soothing and effective.
Fenugreek (Middle East) – Fenugreek, a herb commonly used in Middle Eastern cuisine, has gained popularity as a natural remedy to support lactation. It’s believed that fenugreek can enhance milk production and prevent blocked ducts. Many lactating individuals incorporate fenugreek seeds or supplements into their diets to promote breast health. However, it’s important to use fenugreek under the guidance of a healthcare professional, as its effects can vary from person to person.
Castor Oil Packs (Caribbean) – Castor oil packs have been used as a traditional remedy in India for various ailments, including mastitis. Applying castor oil-soaked cloths or compresses to the affected breast can promote blood circulation, reduce inflammation, and alleviate discomfort. Castor oil is believed to have anti-inflammatory properties that may aid in the healing process. It’s worth noting that while this remedy has historical use, scientific research on its efficacy for mastitis is limited.
Moringa (Africa) – Moringa, a nutrient-rich plant native to Africa, has been utilized for its potential benefits in supporting lactation. Moringa leaves are rich in vitamins, minerals, and antioxidants, making them a valuable addition to the diet of breastfeeding individuals. While there’s limited scientific research specifically on moringa’s role in preventing mastitis, its nutritional profile suggests potential benefits for overall breast health and lactation.
- Frequently Asked Questions
Can mastitis occur even if I’m not breastfeeding?
Mastitis is less common in individuals who are not breastfeeding but can still occur. It’s typically associated with other factors such as skin infections, trauma, or underlying health conditions.
Is mastitis a serious medical condition?
Mastitis itself is not usually a serious condition if treated promptly. However, untreated mastitis can lead to complications such as abscess formation. Seeking medical attention and adhering to treatment recommendations are important to prevent complications.
How long does it take for mastitis to resolve with treatment?
With proper treatment, mild cases of mastitis may show improvement within a day or two. More severe cases might take several days to a week to see significant relief. It’s essential to continue treatment as prescribed until symptoms completely subside.
Are herbal remedies safe to use alongside medical treatment?
While some herbal remedies may offer relief, it’s crucial to consult with a healthcare professional before using them, especially if you’re already on prescribed medications. Herbal remedies can interact with medications and affect their efficacy.
Can mastitis affect both breasts simultaneously?
Yes, mastitis can occur in both breasts at the same time. Adequate breast care, proper latch technique, and frequent breastfeeding can help minimize the risk of bilateral mastitis. If you suspect you have mastitis in both breasts, seeking medical attention is advisable for proper diagnosis and treatment.
How do you know if you have mastitis?
The signs of mastitis can be unmistakable. You may experience breast pain, tenderness, swelling, and redness. The affected breast might feel warm to the touch and appear redder than usual. Flu-like symptoms such as fever, chills, and fatigue may also accompany mastitis. If you notice any of these symptoms, especially in conjunction with breastfeeding, it’s advisable to seek medical attention.
Can mastitis go away on its own?
Mastitis usually requires treatment to resolve completely. While mild cases might improve on their own, seeking medical intervention is crucial to prevent the condition from worsening or leading to complications such as abscess formation. With proper treatment and care, mastitis can be managed effectively and symptoms can be alleviated.
What gets rid of mastitis?
Effective mastitis treatment involves antibiotics to clear bacterial infection, pain relievers to ease discomfort, and methods to promote breast drainage. Continued breastfeeding or pumping, warm compresses, and rest can all contribute to getting rid of mastitis. If symptoms persist or worsen, consulting a healthcare professional is recommended.
How can I get rid of mastitis at home?
At home, you can manage mastitis by:
- Taking prescribed antibiotics as directed.
- Applying warm compresses to the affected breast.
- Using over-the-counter pain relievers under medical guidance.
- Continuing to breastfeed or pump frequently to maintain milk flow.
- Ensuring proper breastfeeding techniques to prevent blocked ducts.
- Staying well-hydrated and maintaining a balanced diet.
Does pumping help mastitis?
Yes, pumping can help alleviate mastitis symptoms by ensuring regular breast drainage. Frequent pumping helps prevent milk accumulation, eases discomfort, and promotes healing. Properly emptying the breast can also clear blocked milk ducts, reducing inflammation.
What does the start of mastitis look like?
The onset of mastitis is often marked by breast pain, tenderness, and redness. The affected breast might appear swollen and warmer than usual. Some individuals also experience flu-like symptoms such as fever, chills, and fatigue.
What is the best treatment for mastitis?
The best treatment for mastitis typically involves a combination of antibiotics to target bacterial infection, pain relievers for discomfort, and strategies to promote breast drainage. Continuing to breastfeed or pump, using warm compresses, and maintaining proper breastfeeding techniques are essential components of effective treatment.
Should I pump if I have mastitis?
Yes, pumping is generally recommended if you have mastitis. Frequent breastfeeding or pumping helps maintain milk flow, prevents further milk accumulation, and clears blocked ducts. Proper breast emptying is beneficial for managing mastitis.
What is the first treatment for mastitis?
The primary treatment for mastitis often involves antibiotics to address the bacterial infection causing inflammation. Seeking medical attention for proper diagnosis and prescription is essential. Rest, warm compresses, and pain relief measures can complement antibiotic treatment.
How quickly can mastitis go away?
With proper treatment, mild cases of mastitis can show improvement within a day or two. More severe cases may take several days to a week to see significant relief. Consistently adhering to the prescribed treatment plan is important for a faster recovery.
What is the main cause of mastitis?
Mastitis is primarily caused by bacterial infection, often introduced through cracked or damaged skin on the breast. The most common bacterium responsible for mastitis is Staphylococcus aureus. Hormonal fluctuations and blocked milk ducts can also contribute to mastitis development.
What are the three stages of mastitis?
Mastitis progresses through three stages:
- Engorgement: Swelling and discomfort as milk accumulates in the breast.
- Inflammation: Symptoms intensify, including pain, redness, warmth, and flu-like symptoms.
- Abscess Formation (if untreated): A pocket of pus forms within the breast, often requiring medical drainage.
What can be mistaken for mastitis?
Other conditions such as a plugged milk duct, breast engorgement, or even a breast abscess can be mistaken for mastitis due to similar symptoms. Consulting a healthcare professional can help differentiate between these conditions.
What does the beginning of mastitis feel like?
At the onset, mastitis can feel like breast tenderness, discomfort, and mild swelling. Some individuals also experience localized warmth and redness in the affected area. These symptoms may progress over time if left untreated.
What comes first with mastitis?
Mastitis typically begins with breast tenderness and discomfort, often accompanied by flu-like symptoms such as fever and fatigue. Redness and warmth in the affected area may follow, and if left untreated, it can lead to abscess formation.
How can I prevent mastitis?
Preventing mastitis involves:
- Ensuring proper latch technique during breastfeeding.
- Emptying breasts regularly through breastfeeding or pumping.
- Wearing comfortable, breathable clothing.
- Addressing cracked or damaged nipples promptly.
- Staying hydrated and maintaining a balanced diet.
- Avoiding unnecessary pressure on the breasts.
What bacteria causes mastitis?
The primary bacterium responsible for mastitis is Staphylococcus aureus. This bacterium can enter the breast through cracks or openings in the skin, leading to localized infection and inflammation.
What is the onset of mastitis?
The onset of mastitis is marked by breast tenderness, discomfort, and swelling. Redness and warmth in the affected area, along with flu-like symptoms, may follow. Timely intervention can prevent the condition from progressing.
How common is mastitis?
Mastitis is relatively common among lactating individuals, especially during the early stages of breastfeeding. It’s estimated that around 10% of breastfeeding individuals will experience mastitis at some point. Early recognition and proper management are key to a successful recovery.