Table of Contents
Spinal Stenosis
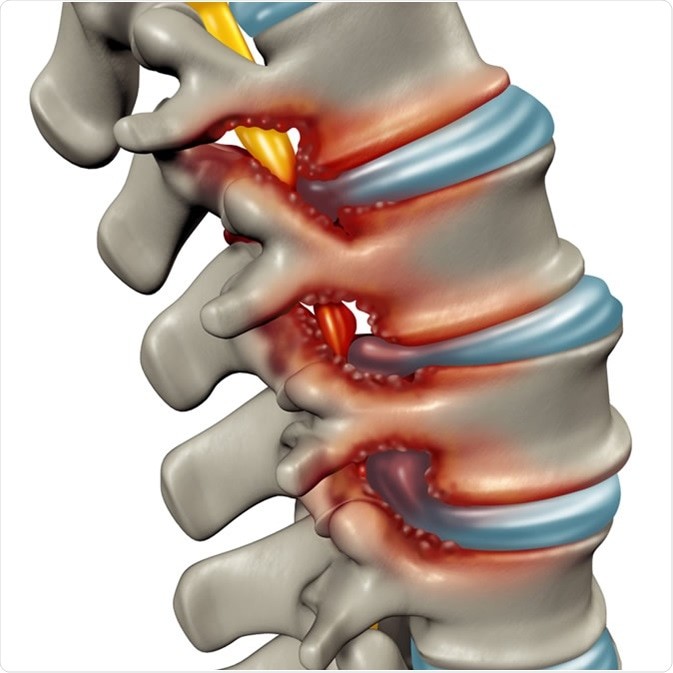
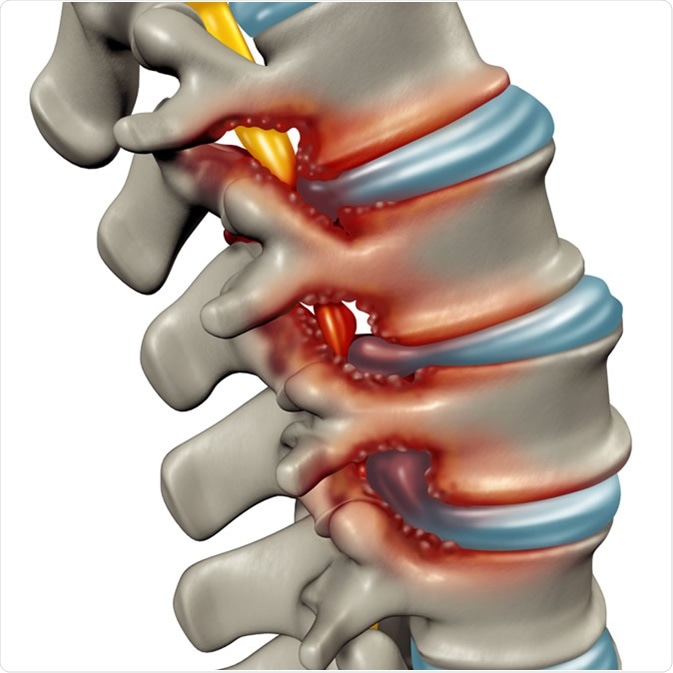
You have spinal stenosis when your spinal canal, in which passes the spinal cord, becomes narrowed. The narrowing causes an abnormal passage of the nerve roots within the spine and leads to their progressive compression. In other words, spinal stenosis occurs when the spinal cord and spinal nerve roots squeeze together.
Although it can affect people of all ages, spinal stenosis is most often related to aging; it is more frequent in people who are in their sixties.
Spinal stenosis may affect different parts of your spine: cervical (cervical stenosis), thoracic (thoracic spinal stenosis) or lumbar (lumbar stenosis). Depending on its location and its severity in your spine, spinal stenosis may cause pain in your back, neck and legs when you walk or stay standing still. The disease can cause severe lower back and leg pain. In severe cases, spinal stenosis can even lead to trouble walking. In some cases, a spinal stenosis can cause painful inflammation in the lumbar vertebrae.
Types of Spinal Stenosis
 In general, there are two main types of spinal stenosis: lumbar stenosis and cervical stenosis.
In general, there are two main types of spinal stenosis: lumbar stenosis and cervical stenosis.
Cervical stenosis – this type of spinal stenosis occurs when the spinal canal is narrowed, causing the nerves to become squeezed and irritated. The narrowing leads to an obstruction of the cerebrospinal fluid (a biologic fluid presents around the brain and spinal cord of the central nervous system), which lead to a variety of symptoms including tingling, numbness, severe pain and sometimes paralysis.
Lumbar stenosis – Lumbar stenosis is a form of spinal stenosis caused by a progressive narrowing of the spinal canal, precisely in the lumbar area. This narrowing often results from a degenerative arthritis of the spine joints, which leads to a reduced size of the spinal canal in the lower back. This condition is more common among the middle-aged and elderly population.
Causes and Risk factors
The two main risk factors of spinal stenosis include age and skeletal fluorosis
Age – age does not cause spinal stenosis; however, as you get older (50 -60 years), your risk of developing spinal stenosis increases considerably.
Skeletal fluorosis – skeletal fluorosis is a condition that results from excessive accumulation of fluoride in the bone, leading to changes in bone structure and making them extremely fragile and brittle (osteogenesis imperfecta). If you have skeletal fluorosis, you are likely to have spinal stenosis.
Spinal Stenosis Symptoms
Spinal stenosis may remain totally asymptomatic for years in some people; some, however, can experience mild pain or cramping in the legs, back, neck or/and shoulders. In some patients, the pain can be so severe that they barely able to walk.
It is not entirely clear how stenosis causes painful symptoms. Researchers believe that the pain in the legs, which are a common symptom of lumbar spinal stenosis, may be the result of compression of small blood vessels providing blood flow to the spinal nerve roots. It is also believed that symptoms of spinal stenosis can be due to direct physical compression of the nerve roots.
In general, if you have spinal stenosis, you will experience pain or numbness in your arms, neck, shoulders, back, legs, and sometimes in your feet. The pain may be accompanied by cramps and aggravated by walking. The pain is often much calmer when you sit or when you bend forward. In addition, you can also have back pain that can be very severe sometimes.
Complications
If you have spinal stenosis, it is not uncommon for you to lose balance from time to time. The disease can put so much pressure on the nerves that control your balance that it impairs your motor coordination in daily activities. You also may experience urinary or fecal incontinence. In severe cases, spinal stenosis may lead to permanent or temporary loss of feeling in your arms, hands, feet or legs.
Spinal Stenosis Causes
Your spine plays a variety of roles in your body functions; it protects the spinal cord, and supports your head and transmits the weight of your body to your hip joints, allowing you walk and stand up straight. Your spine has many joints, which allows mobility of your head, bending your neck and back.
The spine is often called the backbone of the human body. It is composed of 24 vertebrae: 7 cervical, 12 thoracic and 5 lumbar. Between each vertebra is an intervertebral discs (or intervertebral fibrocartilage) made of cartilage that absorbs shock and protects the spinal cord from injuries. The vertebrae are connected together by a series of ligaments. In the center of the spine located the spinal cord which contains nerve cells that process and transmit information, by electrochemical signals, to your brain and different organs of the body.
Spinal stenosis occurs when the spinal canal narrows and compresses the spinal cord and the nerves it contains. This condition is often linked to age; most spinal stenosis patients are over 50 years old. The cause of this degeneration may be “congenital or” developmental “, or a combination of both. However, spinal stenosis is often acquired and is due a degenerative of the intervertebral discs, cartilaginous joints that allow slight movement of the vertebrae. In some cases, acquired degeneration can be added to a congenital spinal problem to give rise to spinal stenosis.
Although rare, the following factors can contribute in the development of stenosis:
- herniated disk
- intradural spinal cord tumors
- injury to spine and spinal cord
- degenerative changes in the ligaments
- achondroplasia – a genetic disorder of bone growth
- amyloidosis – abnormal amyloid deposits in organs and/or tissues
- Paget’s disease of bone – chronic disease of the skeleton characterized by enlarged and deformed bones
- calcium pyrophosphate deposition disease (CPDD) – deposition of calcium pyrophosphate dihydrate (CPPD) in and around joints.
Diagnosis
Usually, the diagnosis of spinal stenosis begins with a complete analysis of your medical history and thorough physical examination. Your doctor will do the physical exam to search and analyze the symptoms being present, and other signs indicating a complication of the disease. In addition, your physician may inquire about the period during which the symptoms occur
The physical exam is also important to determine the severity of the spinal stenosis and assess whether it leads to sensations of cramping or numbness in parts of your body. In addition, neurological assessment can be performed to detect if you have sensation problems. A lack of sensation in your lower body part is tangible evidence of a chronic compression of nerve roots caused by spinal stenosis.
No laboratory analysis can detect the presence or absence of stenosis, however, specific tests may help confirm a malfunction of the nerve roots and spinal cord. In general, tests such as spinal X-ray, MRI, CT scan, CT myelogram, and bone scan. Those procedures are performed not only to discover the disease but also to determining the severity of the degeneration in the spine.
Spinal X-ray – a spinal x-ray is photograph of the skeletal anatomy that is generated using a radioactive material. It is necessary not only to put in evidence a spinal stenosis but also to rule out certain anomalies in the spine such as fractures and bone tumor. However, an x-ray of the lumbar vertebrae can show only the bony structures; intervertebral discs, spinal cord and spinal nerves are not visible. More tests such as MRI and CT scan are needed.
MRI – a magnetic resonance imaging (MRI) is a procedure consist of using magnetic field and radio waves to provide two-dimensional images of the anatomy of soft tissues. This exam is more sophisticated than a standard x-ray and provides more accurate results. Unlike the standard spinal x-ray, the MRI can show not only fracture or bone tumor but also bony structures. Intervertebral discs, spinal cord and spinal nerves can also be examined using this imaging technique.
CT scan – CT examination allows your doctor to visualize very precisely the morphology (shape and size) of the spinal canal and evaluate the impact of the stenosis in your spinal canal.
CT myelogram – a myelogram is a radiographic exam of the spinal canal and nerve roots using special dye and an X-ray. It allows your health care provider to determine the severity of the stenosis, and confirm or rule out presence of herniated disks, bone spurs and tumors.
Bone scan – a bone scan is a procedure that allows your physician to generate images of the skeletal anatomy. During the procedure, your physician injects inside a vein in your arm a radioactive material (radiotracer) in small quantities. Once in your system, the radiotracer attaches to your organs or tissues. Using a special camera called a gamma camera (scintillation camera), your physician may register the radiation emitted by the organ or tissue, allowing him to have multiple images of the part of the body diagnosed.
Lumbar puncture – this procedure is often performed in spinal stenosis diagnosis to obtain information about the cerebrospinal fluid (CSF). Usually, a specialist introduces a needle inside the spine to remove cerebrospinal fluid to be examined in laboratory. The procedure also allows him to inject drugs or a radioactive product to highlight lesions (using an x-ray).
Electromyogram (EMG) – this test is performed to examine the response of a muscle to nerve stimulation. It consists at recording the spontaneous electrical activity of a muscle during contraction. The EMG can study both the muscles and nerves. The collection of information is done through a very thin needle inserted into the muscle and connected to the recording device. During the procedure, your health care provider stimulates a nerve using electrical pulses of very low intensity, and measures the velocity and amplitude of the response through electrodes placed on the skin and connected to a recording machine.
Other tests – depending on the results of those tests, your doctor can collect fluids, such as blood, for analysis purpose. Usually, fluid analysis is recommended to detect problems not revealed by other tests.
Spinal Stenosis Treatment
Most of the times, spinal stenosis is treated effectively with conservative treatments including analgesics, physiotherapy and steroids. Conservative treatments are appropriate in cases of stenosis with mild to moderate symptoms; treatments aim to prevent or control the progression of symptoms and make your life better. If you have severe or spinal stenosis associated with inability or difficulty to walk, your health care provider will consider surgical intervention. In general, spinal stenosis treatment can be nonsurgical or surgical.
Nonsurgical
Nonsteroidal anti-inflammatory drugs (NSAIDs) – this class of medication includes aspirin, ibuprofen and many other molecules. NSAIDs may be used different ways: oral, rectal or injection; cream, ointment, lotion, etc. Your doctor will consider your condition to prescribe you a dosage and method most appropriate. These drugs act by reducing pain, fever and inflammation.
Back brace – this device provides support to the motion of the spine, and enhances the healing process. In addition, back brace can minimize pain and discomfort in your lower back.
Physical therapy – physical therapy is a technique performed by a physiotherapist to treat various muscular and skeletal problems. It can help you develop, maintain and restore movement and functional use of different parts of your body, mostly flexibility of your spine.
Herbal supplements – although their effectiveness is not fully proven, you can take the following supplements to improve your mobility: devil’s claw, burdock, ginger root, turmeric root extract, chondroitin sulfate and glucosamine.
Injection
Epidural steroid injection (ESI) – to reduce your pain, your physician may inject analgesics and steroids into your epidural space, the anatomic structure surrounding the spinal column. To be more effective, your health care provider will use a fluoroscopy to guide the injection directly to the affected nerve roots.
Surgical treatment
The main goal of the surgical treatment of spinal stenosis is to reduce symptoms and improve the quality of your life. Usually, your physician will perform a surgery after a long period (usually six months) of failure of the conservative treatments. Some complications of spinal stenosis that may require surgery include:
- neurogenic claudication
- weakness and numbness of lower limbs
- ineffectiveness of the other treatment to reduce or eliminate symptoms
- lumbago (lower back pain) and leg pains that reduce your daily activities and impact on the quality of your life.
Decompressive laminectomy – this is a surgical procedure to delete all of the lamina and/or thickened tissue. The goal of the surgery is to restore the function of the spinal canal, unsqueeze the spinal cord and nerve roots, and hopefully relieve pain associated with the spinal stenosis. A decompressive laminectomy can be performed anywhere along the spine from the neck to the lower back.
Laminotomy – unlike decompressive laminectomy, laminotomy consist of removing a part of the lamina (thin layer of bone, membrane, or other tissue). A laminectomy allows your surgeon to address the spinal canal and its entire contents. In addition to spinal stenosis, this operation can be performed to treat lumbar spinal stenosis of congenital origin, herniated disc, bone fracture and different nerve compression syndromes.
Arthrodesis – also called spinal fusion, arthrodesis is a surgical procedure performed to permanently block two or more vertebrae together. It is often a non-reversible operation. This procedure requires a bone graft created between the two bones, which can be obtained from your own body (autograft) or from a donor (allograft). The aim of the operation is to correct a deformity or obtain indolence.
Spinal Stenosis Prevention
The main risk factor of spinal stenosis is aging. As you get older, there are changes that naturally occur in your spine that tends to squeeze the spinal cord and its nerve roots. You cannot prevent aging; however, there are steps you can take to minimize your risk of developing spinal stenosis:
- Lift heavy weight with precaution
- Sit comfortably by keeping your spine straight
- Lose weight if you are obese or overweight
- Exercise regularly – that also helps you lose weight
- Adopt a good position when you drive
- If you already have spinal stenosis, wear low-heeled shoes
- Quit or do not smoke – besides cancer and cardiovascular disease, smoking can cause back pain, disc problems, and low bone density
- Spinal stenosis cause weakness and numbness in the legs, which often leads to loss of balance; therefore, avoid alcohol and sedative drugs that increase your risk of losing your balance.
References:
1 – medicalorama.com, Sténose spinale lombaire (ou canal lombaire étroit)
2 – nfra.net, National Fibromyalgia Research Association, Cervical Spinal Stenosis
3 – aafp.org, American Academy of Family Physicians: Lumbar Spine Stenosis: A Common Cause of Back and Leg Pain JAMIE A. ALVAREZ, M.D., and RUSSELL H. HARDY, JR., M.D.
4 – uncorpshumain.com, Seimon, Leaonard P. Low Back Pain: Clinical Diagnosis & Management. Norwalk: Appleton-Century-Crofts, 1983.
5 – mayoclinic.com, Tests and diagnosis
6 – santea.com, EMG ou Électromyogramme
7 – atlasducorpshumain.fr, tests relatifs aux problèmes spinaux
stacommunications.com, Journee de neurolgie ; La sténose spinale lombaire : évaluation et traitement chirurgical minimalement invasif
8 – Fast Facts About Spinal Stenosis”. Niams.nih.gov. Retrieved 2015-04-17.
9 – Meyer F, Börm W, Thomé C; Börm; Thomé (May 2008). “Degenerative cervical spinal stenosis: current strategies in diagnosis and treatment”. Dtsch Arztebl Int 105 (20): 366–72. doi:10.3238/arztebl.2008.0366. PMC 2696878. PMID 19626174.
10 – Wu, Jau-Ching; Ko, Chin-Chu; Yen, Yu-Shu; Huang, Wen-Cheng; Chen, Yu-Chun; Liu, Laura; Tu, Tsung-Hsi; Lo, Su-Shun; Cheng, Henrich (2013-07-01). “Epidemiology of cervical spondylotic myelopathy and its risk of causing spinal cord injury: a national cohort study”. Neurosurgical Focus 35 (1): E10. doi:10.3171/2013.4.FOCUS13122
11 –“Spinal Stenosis Details”. Spinalstenosis.org. Retrieved May 27, 2016.
12 – Treatment of Degenerative Lumbar Spinal Stenosis, Evidence Report/Technology Assessment, No. 32]. (2001). In AHRQ Archive. May 27, 2016.
13 – Malamut, edited by Joseph I. Sirven, Barbara L. (2008). Clinical neurology of the older adult (2nd ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 220. ISBN 9780781769471.
14 – “coflex Interlaminar Technology – P110008”. Fda.gov. 2014-01-17. Retrieved 2015-04-17.
14 – http://web.archive.org/web/20130522092317/http://www.vancouverspinecarecentre.com/con_spinalstenosis. Archived from the original on May 22, 2013.
15 – Cluett, Jonathan, M.D. (2010) Spinal Stenosis – How is Spinal Stenosis Diagnosed?
16 – Zaina, F; Tomkins-Lane, C; Carragee, E; Negrini, S (29 January 2016). “Surgical versus non-surgical treatment for lumbar spinal stenosis.”. The Cochrane database of systematic reviews 1: CD010264. doi:10.1002/14651858.CD010264.pub2. PMID 26824399. Retrieved 5 February 2016.