Table of Contents
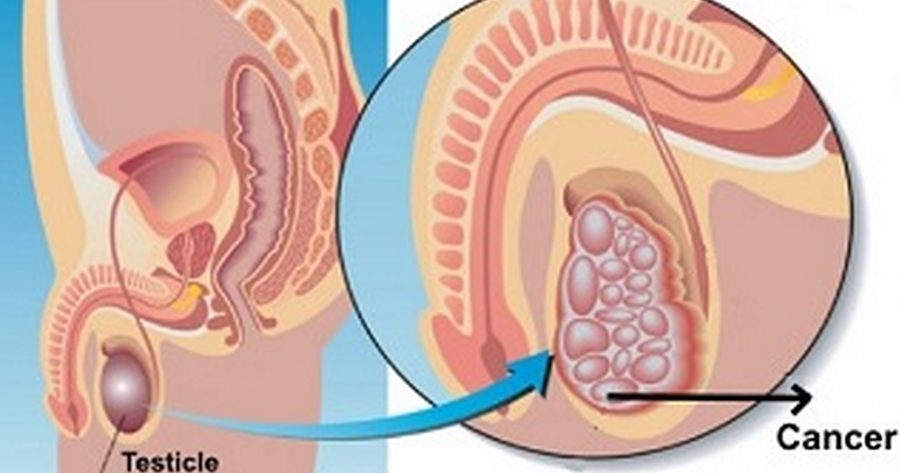
Testicular cancer is a malignant tumor that starts in the cells of the testicle. In other words, when you have testicular cancer, you have an uncontrolled growth of malignant cells in one or both of your testicles. Unlike many cancers, testicular cancer responds well to medical treatment; however, the therapies (surgery, radiotherapy and chemotherapy) often lead to infertility.
Depending on the group of cells affected, testicular cancer are grouped into two broad categories: seminoma testicular cancer and nonseminoma testicular cancer.
- Seminomais more common in older men, and tends to have a good prognosis. The tumor grows slowly and responds well to radiation therapy.
- Nonseminoma, in the other hands, grows quickly, and tends to be very aggressive. Unlike the seminoma, nonseminoma testicular canceris not sensitive to radiotherapy. Seminoma testicular cancer includesseveralsubtypes:
- teratocarcinoma, represent about 30% of testicular cancer
- embryonal carcinoma, account for 20% of testicular cancer
- Choriocarcinoma, the rarest and highly malignant form of testicular cancer.
Testicular Cancer Incidence
Testicular cancer is rare in the world, especially among black men. It accounts for 1 to 2% of men cancers, and less than 4% of urologic tumors. The malignancy affects about 1 in 20 000 men. However, testicular cancer is the most common cancer in young men, particularly males who are in their mid-twenties.
From 2002-2006, the highest incidence of testicular cancer was registered among male aged between 20 and 34. Percentages and ages of men diagnosed with testicular cancer were approximately:
- 5% under age 20;
- 6% between 20 and 34;
- 9% between 35 and 44;
- 5% between 45 and 54;
- 5% between 55 and 64;
- 1% between 65 and 74;
- 6% between 75 and 84;
- 2% 85+ years of age.
Worldwide, approximately 49 000 men are diagnosed with testicular cancer each year. In the United States, about 8,000 testicular cancer cases are registered each year. According to the National Cancer Institute (NCI), it is estimated that 8,400 men were diagnosed with cancer of the testis in 2009; 380 died of it.
Testicular cancer Causes
The testes are two male sex glands located outside the pelvis into the scrotum. They are fixed to the scrotum by the spermatic cord, the structure of the male genitalia containing the vas deferens, some lymph nodes, veins and nerves. Each adult testis measures approximately 14 cm³ – 35 cm³ with a weight of about 18 g. The two main roles of the testicles are to produce sperm, which then pass through the vas deferens to reach the prostate in which it mixes with seminal fluid to form semen; and synthesize male hormones including testosterone.
All these features are possible thanks to thousands of cells working in synergy. Every day, thousands of testicular cells die (self-cell destruction or apoptosis) to be replaced by new healthy cells. Testicular cancer occurs when there is abnormal and anomic cell proliferation in the testes. The testes become assailed by cells which multiply exaggeratedly without committing suicide.
The cause of this cellular disorder is not well known; risk factors, however, are suspected.
Testicular Cancer Risk Factors
The exact cause of testicular cancer is not well known, but several factors are suspected in the development of the disease. Most common factors that may increase your chance of having testicular cancer include:
- Age– testicular cancer is more common among men aged 15 to 34 years old, and is very rare before age 15 and after age 50.
- Race– Testicular cancer is more common among white men than those of African origin.
- HIV/Aids– risk of testicular cancer is higher among victims of HIV/Aids.
- Family history –if your family members have a history of testicular cancer, you have an increased risk of having it.
- Testicular atrophy– a decrease in the testes volume, especially after mumps or after a trauma, appears to increase the risk of testicular cancer significantly.
- Ectopic or undescended testicle– an undescended testicle (one or both testicles fail to move
into the scrotum before birth) in childhood is considered as the greatest risk factor of testicular cancer.
Testicular Cancer Symptoms

Unlike many cancers, testicular cancer can be detected in its early stage with no sophisticated medical exams. Most of the times, the tumor manifests by a mass in one or both testicles. That is why it is necessary for all men to regular do a testicular self-examination. The exam is recommended to be done after a hot shower or bath, because the scrotum is looser. If you find a hard part or the entire testicle is hard and bumpy to the touch, it is important to contact your urologist; it may be a testicular cancer.
In general, testicular cancer symptoms include at least one of the following:
- Presence of blood in semen
- lack of sexual desire or interest
- abnormal sensitivity to the touch
- general weakness and tired feeling
- Enlargement or tenderness of the breasts
- a lump in one testis or a hardening of one of the testicles
- A burning sensation, specially following physical activity
- build-up of fluid in the scrotum or tunica vaginalis(hydrocele)
- lower back pain characterized by a dull ache in the lower abdomen or groin
- Sudden or inexplicable change in the size of one or both testes.
Testicular Cancer Complications
Testicular cancer rarely causes complications, but the treatment does. Radiation therapy can cause erectile dysfunction which can last a lifetime, especially in older men. Chemotherapy, although rare, can lead to permanent erectile dysfunction, and can cause infertility.
Men with testicular cancer and have lost their sexual desire often have psychological problems. These problems may be due to the fact that they cannot enjoy their sex life.
In addition, men who already had testicular cancer are at increased risk of developing leukemia and other cancers.
Testicular Cancer Diagnosis
If you examine your testicles regularly, you may suspect the cancer by yourself. However, to confirm the diagnosis, you will need the help of a medical professional. Your doctor will do a physical exam and ask you question about your medical history. It is likely that your doctor suspect the cancer after the interrogation and the physical exam.
However, to accurately confirm that you have testicular cancer, your doctor will recommend blood tests, imaging techniques and biopsy.
Ultrasound – an ultrasound of the scrotum is the imaging technique of choice for evaluating problems linked testicular cancer. Your doctor will recommend this test if, during the physical examination, he noticed a swelling in the scrotum which indicates presence of a tumor.
Ultrasonography of the scrotum allows your doctor to evaluate the testis and epididymis (the tube that collects sperm produced in the testicles), and to determine whether you have cancer or another health problem having symptoms similar to testicular cancer: inflammation of the scrotum, undescended or absent testicle, testicular torsion or abnormal blood vessels in the testes.
Blood tests – an analysis of your blood will be performed to verify the amount and appearance of different types of blood cells, and thus the functioning of your organs, including testes. In addition, blood analysis can provide evidence suggesting the presence or absence of cancer in your testicles.
The main goal of the blood test is to find some chemical substances called tumor markers specific to testicular cancer. In general, in the diagnosis of your testicular cancer, your health care provider will seek the AFP (alpha-fetoprotein or alpha-1-fetoprotein), HCG (beta-human chorionic gonadotropin) and LDH (lactate dehydrogenase).
Orchiectomy and biopsy – other procedures may indicate the presence of cancer in your testicles, but only a biopsy can confirm the presence of cancerous cells. Usually, to make possible the biopsy, your surgeon will perform an orchiectomy, complete removal of the diseased testicle. The intervention will be performed in hospital, under general anesthesia. The testicle removed will be examined in the laboratory to determine if the lump is cancerous or not. If the diagnosis is confirmed, your doctor will also seek to determine the type of cancer you have in order to choose the most appropriate treatment to fight the tumor.
Testicular Cancer Stages
Once the cancer is found in your testicle, your doctor will perform some test to determine its stage; he will recommend a chest and abdominal CT scan and a chest x-ray. The x-ray can show if the cancer has invaded the lungs, whereas the CT scan will provide information about the spreading of the cancer into lymph nodes in the abdomen. In addition, your doctor may recommend an intravenous pyelogram (IVP) to explore the urinary tract; and a lymphangiography, which allows him to visualize the lymphatic system.
In general, testicular cancer evolves in three stages:
- Stade I– the cancer is still limited to testicle;
- Stade II– the cancer has invaded the abdominal lymph nodes;
- Stage III –the cancer has reached nearby lymph nodes and other parts of the body: lungs, liver, bones or brain
- Recurrence: the cancer has returned after treatment.
Testicular Cancer Treatment
Knowing your age, medical condition and the type and stage of your cancer, your doctor will determine the most appropriate and effective treatment for your condition. After all, you will be invited to participate in the final choice.
Unlike many other cancers, testicular cancer can be permanently cured. The most common treatment for testicular cancer includes surgery, chemotherapy and radiotherapy.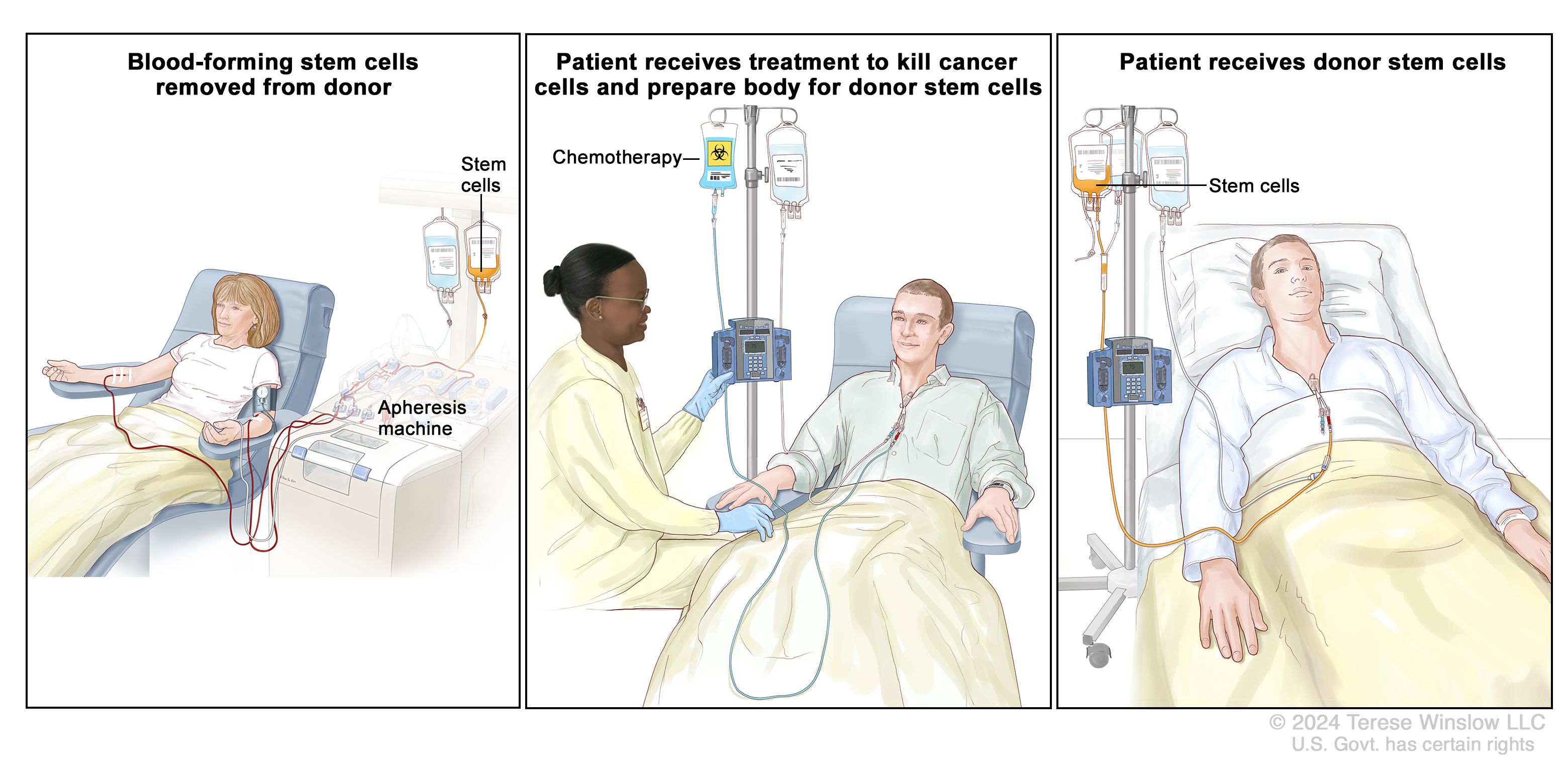
Surgical treatment
Orchiectomy – removal of the diseased testis by inguinal surgery is always the first therapeutic step your doctor will take to get rid of the cancer. Because only one testicle is often affected, surgery is very often performed to remove one testicle. Surgery may be the only treatment used if you have an early stage testicular cancer; in moderate or advanced testicular cancer, the surgery can be associated with other therapies.
Unlike chemotherapy and radiotherapy, orchiectomy does not usually cause fertility or erectile dysfunction. For aesthetic reasons, a testicular prosthesis of the same size as the opposite testicle can be implemented.
Removal of lymph nodes – in advanced testicular cancer, your surgeon can perform a removal of abdominal lymph nodes after the first operation or after chemotherapy to eliminate the cancer completely and reduce the chances of recurrence. Although it does not cause erection problems, this procedure can cause permanent infertility.
Regular monitoring – after surgery, you will be advised to see your doctor regularly during the following years. You will be recommended to do blood tests, CT scans and X-ray examinations in order to monitor the tumor closely. In case of recurrence, your oncologist will use radiotherapy, chemotherapy or a combination of both to fight the cancer.
Chemotherapy
If you were diagnosed with advanced testicular cancer, your oncologist can recommend you to take chemotherapy drugs. Chemotherapy is a cancer treatment consists of using powerful chemical agents to destroy cancerous cells. These drugs can be administered orally or intravenously. Depending on the characteristic of the tumor, you can be prescribed monochemotherapy (single chemical agent) or polychemotherapy (two or more chemotherapy agents).
Chemotherapy is used in the treatment of testicular cancer if the tumor has spread to other sites, particularly lymph nodes. Because chemotherapy attacks both cancerous cells and healthy cells, it can cause several side effects:
- nausea and vomiting
- fatigue
- weakness
- hair Loss
- infertility
- decreased appetite
- Increased risk of infection.
Radiation therapy (Radiotherapy)
During the radiation therapy, your physician will expose the diseased testicle to ionizing radiation in order to alter the composition of the genetic information of the cancer cells. Unlike chemotherapy, radiation acts locally on the region that is irradiated, thereby limits its action to the tumor and a small amount of healthy surrounding tissue.
Radiotherapy can be used before or after surgery, alone or in combination with surgery. Radiation therapy shrinks the tumor and prevents it from spreading into lymph nodes in the abdomen in case of seminoma. However, radiotherapy can cause temporary or permanent infertility.
Semen preservation
Since radiotherapy can cause infertility, your oncologist can preserve your sperm, if you want to have children in the future. Talk to your doctor for more information on semen preservation.
Testicular Cancer Prognosis
Testicular cancer responds well to medical treatment, which makes about 95% of patients survive years after the treatment. In fact, complete recovery from testicular cancer diagnosed early is 100 percent. Even in advanced testicular cancer, where the tumor has spread into nearby lymph nodes, chemotherapy can offer a cure rate of at least 85 percent.
The age-adjusted death rate, based on patients who died in 2002-2006 in the US, was 0.3 per 100,000 men per year. The overall 5-year relative survival rate for 1999-2005 was 95.3%. Five-year relative survival rates by race were approximately:
- 6% for white men
- 4% for black men.
Testicular Cancer Prevention
The fact that no cause of testicular cancer is clearly known, it is difficult to establish a sure preventive method. The best decision is to catch the cancer at an early stage. To do so, you need to practice monthly self-examination of your testicles from age 15, and throughout your life. The exam is easier when the skin of the scrotum is relaxed after a warm bath or shower.
The monthly self-examination of your testicles is not difficult; here is a very easy method that can guide you:
- Stand before a mirror; search for any swelling of the skin of your scrotum.
- Hold your scrotum in your hands in a manner to feel the size and weight of each testicle. It is likely that one of your testicles is larger or descends lower than the other one; this is normal.
- Feel each testicle and roll it between your thumb and finger; it should be smooth. You should feel a soft and sensitive cord in the back of each testicle. You should feel no pain.
- If you notice any of these changes below, contact your doctor as soon as possible:
- a hard mass – as a pea;
- any change in the size, shape,
- sensitivity to touch or painful feeling in the testicles or scrotum;
- swollen testicles or scrotum;
- pain in the testicles or scrotum;
In addition, it is important to talk to your doctor if you experience any of these symptoms for several days:
- unreasonable weight loss
- dull ache or heaviness in the lower abdomen
- abnormal and persistent lower back pain
- An increase in breast size.