Table of Contents
The red liquid in the toilet should be a warning. For most people, spotting blood in their urine is unsettling enough to make them pick up the phone and call a doctor. The most common first sign that something is dangerously wrong. But for roughly one in twelve men, and one in two hundred women, this vivid alarm bell never registers.
They see brown. They see rust. They see darkness. They don’t see red.
This is the peculiar tragedy at the heart of a study published this month in Nature Health: people with color vision deficiency (a common inherited condition affecting roughly eight percent of men worldwide) who develop bladder cancer face a starkly different fate than their peers with normal sight. Over twenty years, they die at fifty-two percent higher rates.
It sounds like a statistical artifact, a rounding error in the epidemiological noise. But buried in that number is a cascade of delayed diagnoses, more aggressive disease, and opportunities lost in the seconds it takes to recognize a color that simply doesn’t exist in your visual world.
The unseen symptom
Bladder cancer is the fourth most common cancer among men in the United States. Nearly 85,000 Americans received the diagnosis in 2025 alone. In the vast majority of cases, somewhere between eighty and ninety percent, the first sign arrives quietly: painless blood in the urine. Without pain. Without other warning. Just that telltale discoloration that sends people racing to seek help.
Except when they can’t see it.
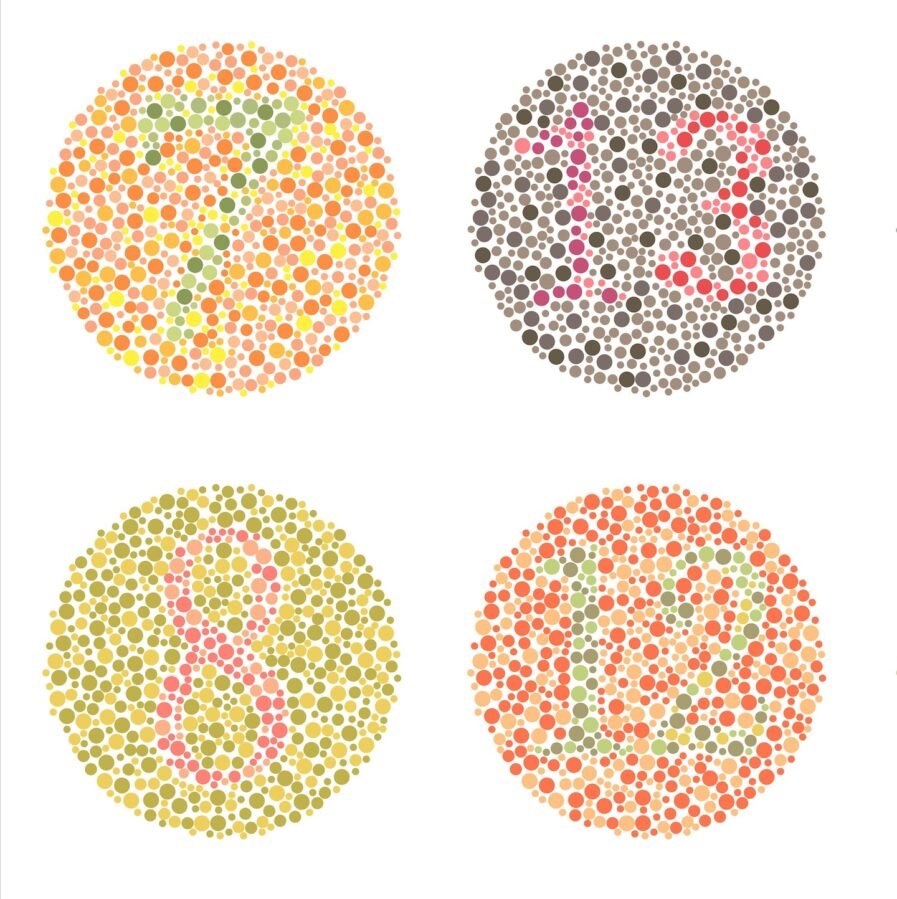
The mechanics of red-green colorblindness are straightforward enough. The inherited condition affects the photoreceptor cells in the retina, impairing the ability to distinguish between red and green wavelengths. It’s an inconvenience in everyday life. Deciphering traffic lights, matching clothes, judging the doneness of meat on a plate. But for bladder cancer, it becomes something far more serious.
In 2001, researchers conducted a deceptively simple experiment. They showed photographs of saliva, urine, and stool to two groups: people with normal color vision and people who were colorblind. Identify which ones contained blood, they asked. The control group got it right ninety-nine percent of the time. The colorblind participants? Seventy percent. A gap wide enough that it might cost you your life.
By 2009, urologists examining a smaller cohort of two hundred men with bladder cancer noticed something troubling. The colorblind patients arrived at their clinics with more invasive disease. They weren’t catching it early. They were catching it late, when the cancer had already begun invading deeper tissue, when treatment options narrowed and outcomes darkened.
These were hints. Important ones. But they remained fragmented. Case reports and small studies scattered through the medical literature, never quite adding up to a clear signal that clinicians needed to hear.
Finding the rare combination
Mustafa Fattah, a medical student at Columbia University, and his colleagues decided to ask a larger question: does this actually change who survives?
To answer it, they needed a needle-in-a-haystack population. People who were colorblind and had bladder cancer. The combination is statistically uncommon enough that no single hospital, no single city, could muster a meaningful sample. So they turned to TriNetX, a research platform that aggregates real-time electronic health records from around the world. Roughly 275 million patient records, de-identified and accessible for researchers hunting for rare populations.
“The power in this type of study is the ability to curate a particular population of interest. In this case, patients who are colorblind who develop bladder cancer or colorectal cancer,” says Ehsan Rahimy, senior author and an ophthalmologist at Stanford. “It’s unusual to have that combination, but when you’re casting a net in an ocean’s worth of data, you have a better shot at capturing a rare fish.”
They cast that net wide. From roughly 100 million United States patient records, they hauled up 135 people with both colorblindness and bladder cancer. They matched each against a control of similar age, sex, and health profile. But with normal vision. Then they waited, watching survival curves diverge.
The colorblind cohort died at significantly higher rates. Over twenty years, their mortality risk was fifty-two percent higher than their sighted counterparts. In statistical terms: a risk ratio of 1.52, with a P-value of 0.025. In human terms: a gap between life and death, measured in the seconds it takes to notice a color change in a toilet bowl.
The mechanism seemed clear from the literature. Patients with colorblindness were missing the most obvious signal that something was wrong. They delayed seeking care. Sometimes by weeks, sometimes by months, until a spouse or family member noticed what they themselves could not see. That delay allowed cancer cells to invade deeper, to reach more advanced stages, to become harder to treat.
For colorectal cancer, the team found something different. No mortality gap. The same colorblind patients facing the same challenge of not seeing red in the stool, yet their survival rates matched those of sighted patients with the same diagnosis.
Why the difference? Because blood in the stool is rarely the whole story for colorectal cancer. Nearly two-thirds of patients initially complain of abdominal pain. More than half notice changes in bowel habits. The cancer announces itself through multiple channels. And there’s another factor: screening. The United States Preventive Services Task Force recommends that everyone aged forty-five and older undergo regular colonoscopy. Routine screening catches cancers before they’ve become visible in any form. There is no such recommendation for bladder cancer. For bladder cancer, you’re on your own. Relying entirely on noticing that change in color.
The limits of what was counted
Rahimy and his colleagues are cautious about their findings. This is hypothesis-generating work, they emphasize. It should raise clinicians’ suspicion. It should prompt further investigation. But there are cracks in the foundation.
The study relies on ICD-10 diagnostic codes. Standardized classifications that patients and their doctors enter into electronic health records. For colorblindness to show up in the data, someone had to notice it, test for it, and formally code it. But colorblindness is largely invisible. Most people with the condition function perfectly fine. Many never discover they have it. In the United Kingdom, eighty percent of colorblind students remain undiagnosed by the time they reach secondary school. In Latvia, fifty-five percent of people with colorblindness only learned about it in adulthood, usually in an occupational context. The United States has no consistent screening program. Only eleven states require color vision screening in schoolchildren. Only one state requires it for all drivers.
“Most people with color vision deficiency are typically functioning fine,” Rahimy notes. “They don’t have any other vision issues. Many affected individuals may not even know they have it.”
This means the true effect is probably larger than the numbers suggest. Everyone diagnosed with colorblindness who developed bladder cancer made it into the study. But many people with undiagnosed colorblindness. Who had no idea they couldn’t see red properly. Ended up in the control group instead, inadvertently weakening the signal. The fifty-two percent mortality gap may be a conservative estimate of the true risk.
What now?
Rahimy has already heard from urologists and gastroenterologists. Including a colleague who is himself colorblind. They said they had never considered colorblindness as a factor in cancer diagnosis. Some have started asking about it on screening questionnaires. It’s a small change, but it’s something.
“If this study raises awareness and people read this and casually pass it along, I think it’s done its job,” Rahimy says.
For patients with colorblindness, the practical implications are concrete. Get a urine test at every annual checkup. And perhaps ask the person you share your life with to notice what you cannot. To periodically check your urine for the presence of blood, a simple act of attention that could mean the difference between a treatable early-stage cancer and an aggressive late-stage disease.
It’s an unusual accommodation in modern medicine. A step backward to the era when diagnosis relied on observation by others rather than self-monitoring. But sometimes the simplest interventions are the most effective. Sometimes the best technology is another pair of eyes that see what you see. And the colors you don’t.
Sources
Fattah, M., Alsoudi, A.F., Mruthyunjaya, P., & Rahimy, E. (2026). Impact of colour vision deficiency on bladder and colorectal cancer survival. Nature Health, 1, 113-119.
If our reporting has informed or inspired you, please consider making a donation. Every contribution, no matter the size, empowers us to continue delivering accurate, engaging, and trustworthy science and medical news. Independent journalism requires time, effort, and resources—your support ensures we can keep uncovering the stories that matter most to you.
Join us in making knowledge accessible and impactful. Thank you for standing with us!