Table of Contents

A hidden immune cascade linking the gut and bone marrow may explain how IBD turns inflammation into colon cancer.
Scientists at Weill Cornell Medicine have identified a complex immune process in the gut that may help explain why people with inflammatory bowel disease (IBD) face a much higher risk of colorectal cancer. The preclinical study shows how a specific immune signal can trigger a wave of white blood cells from the bone marrow into the gut, creating conditions that support tumor growth. The findings also suggest new approaches for detecting disease activity, tracking risk, and developing future treatments.
The Role of TL1A in Gut Inflammation
The research focused on TL1A, an inflammatory immune signaling protein already known to be linked to both IBD and colorectal cancer. Several experimental drugs that block TL1A have shown strong results in clinical trials for treating IBD. However, scientists had not fully understood how this protein contributes to ongoing inflammation or cancer development.
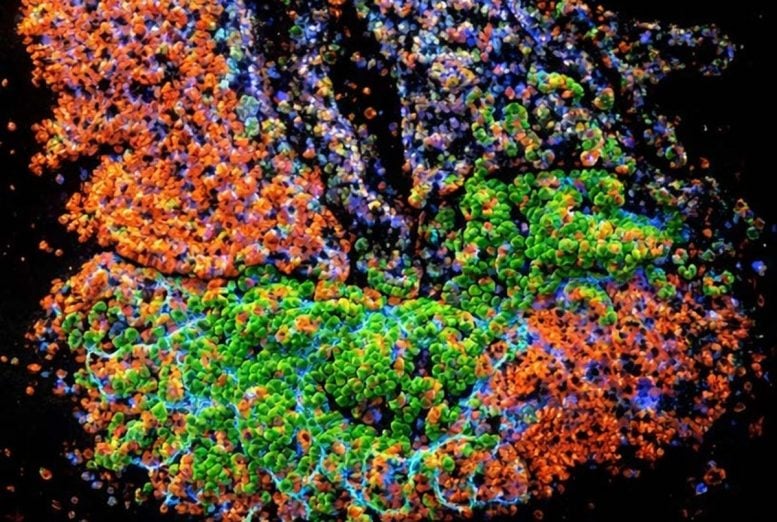
In a study published in Immunity, researchers showed that TL1A exerts much of its effect through immune cells in the gut known as ILC3s. When TL1A activates these cells, they call in large numbers of neutrophils, a type of white blood cell, from the bone marrow. Once recruited, the neutrophils are altered in ways that support tumor formation.
“These findings are important given the intense interest in the medical community to understand TL1A’s role in IBD and its potential role in associated colorectal cancers—for which we have had few strategies to mitigate the cancer risk,” said study senior author Dr. Randy Longman, director of the Jill Roberts Center for Inflammatory Bowel Disease at Weill Cornell Medicine and NewYork-Presbyterian/Weill Cornell Medical Center and an associate professor of medicine at Weill Cornell Medicine.
Why IBD Raises Colorectal Cancer Risk
IBD includes Crohn’s disease and ulcerative colitis and is marked by persistent inflammation in the digestive tract. According to the U.S. Centers for Disease Control and Prevention, between 2.4 and 3.1 million Americans are living with the condition. Beyond digestive symptoms, IBD increases the risk of other autoimmune and inflammatory diseases and greatly raises the likelihood of colorectal cancer. In people with IBD, colorectal cancer often develops at younger ages and is associated with poorer outcomes.
How Gut Cells Trigger Bone Marrow Responses
Dr. Longman’s team found that TL1A is produced mainly by immune cells already present in the inflamed gut of people with IBD. The protein promotes tumor growth primarily by activating ILC3 cells that reside in the intestine. Once activated, these cells release granulocyte-macrophage colony-stimulating factor (GM-CSF), a molecule that stimulates blood cell production.
This signal sets off a process called “emergency granulopoiesis”—a burst of new neutrophil production in bone marrow—followed by the movement of these cells into the gut. In mouse models of intestinal cancer, simply increasing the number of these neutrophils was enough to accelerate tumor development.
Tumor-Promoting Changes in Immune Cells
Neutrophils are known to contribute to colorectal cancer by releasing highly reactive molecules that can damage DNA in the cells lining the intestine. The researchers also discovered that ILC3 cells cause neutrophils to adopt a distinct pattern of gene activity. This pattern includes higher expression of genes linked to tumor initiation and growth.
A similar gene activity signature was found in colon tissue samples from patients with IBD-related colitis. Importantly, this tumor-promoting pattern was less pronounced in patients who had received an experimental treatment that blocks TL1A activity.
New Targets for Future Treatments
The findings suggest that several parts of this immune pathway could become targets for future therapies. In addition to TL1A, ILC3 cells, GM-CSF, and the neutrophils recruited by ILC3s may all play roles in new strategies to treat IBD while also reducing the risk of colorectal cancer.
“I think it will be exciting for clinicians in the IBD field to know that there is a systemic process at work here, involving both the gut and the bone marrow, with the potential to drive precision medicine in IBD,” said study first author Dr. Sílvia Pires, an instructor in medicine and member of the Longman Laboratory.
What Comes Next
The research team is continuing to study this immune communication pathway in the context of gut inflammation. Future work will explore whether early or intermittent exposure to GM-CSF may prime bone marrow cells in ways that increase the likelihood of developing IBD over time, potentially opening new avenues for early intervention and prevention.
Reference: “Innate lymphoid cells activated by the cytokine TL1A link colitis to emergency granulopoiesis and the recruitment of tumor-promoting neutrophils” by Sílvia Pires, Wei Yang, Sofia Frigerio, Cynthia Louis, Chloe Scott, Yu Lin Zhou, Emre Cardakli, Nancy Tran, Mina Hassan-Zahraee, Zhan Ye, Craig Hyde, Kenneth Hung, Amanda Chen, Charles Ng, Alexander Grier, Dana Lukin, Ellen Scherl, Stephan R. Targan, Gretchen E. Diehl, Joep Grootjans, Tracy L. Putoczki, Ian Wicks and Randy S. Longman, 22 January 2026, Immunity.
DOI: 10.1016/j.immuni.2025.12.008
Never miss a breakthrough: Join the SciTechDaily newsletter.
Follow us on Google and Google News.


