Table of Contents
The breast is an exocrine gland that develops during the life of women. It contains the mammary glands which become active during periods of lactation to produce milk. In addition to breastfeeding, the breast plays a vital role in the shape and confidence of a woman. However, the breast is subject to many diseases, among which cancer.
Breast cancer is a malignant tumor that develops in the mammary gland, more especially in the inner lining of the milk ducts. This condition occurs when abnormal cells, under the action of external aggression or carcinogens (such as smoking or ultraviolet rays), multiply anarchically to form a malignant growth.
Without therapeutic intervention, these malignant cells will continue to proliferate, and spread into other tissues in the body to form metastatic cancers; this condition is called metastatic breast cancer. Symptoms or characteristic of metastatic breast cancer depends significantly on the location of a secondary tumor.
Although men also have breast cancer, the disease is more common among women. It is estimated that about one woman out of seven will be affected by breast cancer during their lifetime, which makes the disease the leading cause of death among gynaecological cancers in developed countries.
1. Causes
The breast is an organ composed mainly of fat, glands and milk ducts (also called lactiferous ducts, galactophorous ducts, mammary ducts, or mamillary ducts). During periods of lactation, the glands produce milk, which is transported to the nipple by the ducts. In a healthy breast, cells group together to form tissues. Each tissue works together synchronously and harmoniously to perform a similar function.
The breast tissue is influenced by hormones estrogen and progesterone, two hormones produced by women in variable amounts throughout their lives: puberty, pregnancy, lactation.
Breast cancer occurs when a group of healthy cells begin to transform and divide in an uncontrolled manner to become malignant. If your immune system is robust enough, these tumour cells will be destroyed. Otherwise, these diseased cells continue to multiply to form a malignant tumour (cancer), first limited within the breast; in fact, these cancer cells can remain in the breast asymptomatically for months or years. With time, however, they travel through the lymphatic system or bloodstream to invade other organs distant from the breast to form new tumours called metastases. Despite advances in medical science, the exact causes of breast cancer are still not well known. However, many conditions are suspected in the development of the disease.
For example, immediate family history of breast cancer represents 5-10% risk factor of the disease. In addition, excess weight, diet rich in animal fats, lack of pregnancy, late first pregnancy, early onset of menstruation, late menopause, specific forms of mastopathy (any non malignant disease or pain of the mammary gland), and malignant tumor of the large bowel, uterine or ovaries also seem to contribute in the development of breast cancer.
2. Risk Factors.
About 70% of breast cancer cases occur without any definite cause; a tumour happens without an apparent reason. However, there are factors identified as apparent risks of breast cancer.
Most factors that can increase the risk of breast cancer include:
- Age: although breast cancer can affect young women of all ages, its risk increases with age. It is shown that breast cancer is more common among older people. Therefore, if you are aged 45 or older, your risk of developing breast cancer may be about two times higher than those in their thirties; if you are between 55 and 64, your risk is about three times higher than women in their forties.
- Hormone Replacement Therapy (HRT): according to WHO (World Health Organization), menopause hormone therapy (MHT) is a risk factor for breast cancer especially when taken for more than five years. Some scientists believe that the risk of developing breast cancer increases by 1% per year by taking estrogen alone and 8% per year if the therapy consists of a combination of estrogen and progesterone. Also, studies show that hormone therapy can also increase the risk of colon cancer. However, those risks may disappear about two years after cessation of the treatment.
- Prolonged exposure to endogenous estrogen: in menopause women, this hormone is produced by the body under the action of the adrenal glands. In premenopausal women, it is produced at 60% by the ovaries (estradiol) and 40% by the adrenal glands (estrone). Prolonged exposure to endogenous estrogens may be a risk of breast cancer. It is found mostly amongst women aged 35 to 65 years old who had their first menstruation early (before age 12 for instance), late menopause, nulliparity (no pregnancy) or late pregnancy.
- Family history: your genetic factors of developing breast cancer are about 5-10% if you have close relatives suffering from the disease. Genetic is primarily responsible for breast cancers occurring before age 40.
Some genes that appear responsible for developing the disease include BRCA I, a defect on chromosome 17 associated with an increased risk for breast cancer, and inherited by only 1 in 200 women; and BRCA II, defect on chromosome 13 which is associated with an increased risk of ovarian cancer, fallopian tube cancer, prostate cancer, and pancreatic cancer, as well as malignant melanoma. BRCA II is also associated with breast cancer in men. It is thought that defects in TSG101 (tumour susceptibility gene 101) may have a role in the development of a breast tumour. However, the significance of TSG101 alterations in the development of cancer (carcinogenesis) is controversial since aberrant transcripts of the TSG101 gene have also been identified in normal non-cancerous tissues. - Ataxia-telangiectasia, a rare neurodegenerative disorder, is another inherited disease suspected to weaken the immune system, leading to respiratory ailments and increased risk of breast cancer.
- Nutrition: In addition to its beneficial effect on bone and against chronic pain, vitamin D may play a role in the prevention of the proliferation of cancer cells in women breast. Vitamin A deficiency among female victims of breast cancer seems to contribute to the development of the disease. A group of doctors at Mount Sinai Hospital in Toronto compared the vitamin D levels of 760 women with breast cancer with those of 1 140 healthy women. The studies have shown that high levels of vitamin D were associated with a decrease of 24% risk of breast cancer. In the other hand, it is found that soy products, some fatty acids (mostly omega-3), fruits, cruciferous vegetables and all other natural foods that are rich anti-oxidant vitamins can reduce up to 20% the risk of breast cancer. These substances fight against breast cancer by destroying free radicals and blocking the hormone receptors.
- Smoking: in addition to pulmonary, oral, head and neck cancers, cigarette smoke can also cause breast cancer. Comparably to non-smoker women, Many studies have revealed that the risk of breast cancer before age 50 is about 70% higher among women who start smoking regularly within five years after the onset of their menstruation.
- Alcohol: moderate consumption of alcohol is causative for breast cancer. This risk increases by 9% for each glass of alcohol consumed daily. The contribution of alcohol to the development of breast cancer is mostly in pre-menopausal women and also in postmenopausal women who take hormone replacement.
- X-rays and mammography: the modern mammography equipment delivers very little radiation compared to what existed 15-20 years ago, which lowers its carcinogenic potentiality considerably.
However, the risk of breast cancer exists for women under 30 years due to glandular susceptibility and the fact women of these ages require a more significant amount of radiation for imaging of their breasts. Therefore, repeated mammography can increase the risk of breast cancer in young women. - Puberty and menopause – An early puberty and late menopause can increase the susceptibility to be affected by breast cancer. A woman whose menopause happens naturally after age 55 has more chances to have breast cancer than a woman who has her menopause before age 45.
- Pregnancy – the absence of pregnancy can increase the chances of breast cancer. Also, if you have your first pregnancy in your thirties, you have two times more chances to develop breast cancer over a woman who becomes a mother in her early twenties. The risk is even higher if you have no children.
- Breastfeeding – although some women do not like it, breastfeeding plays a crucial role in preventing breast cancer. Studies have shown that prolonged breastfeeding reduces the risk of developing breast cancer considerably. Also, it provides many benefits in the physical and mental development of the infant. By breastfeeding you increase the chance of your infant to be healthy, and decrease your risk of developing breast cancer.
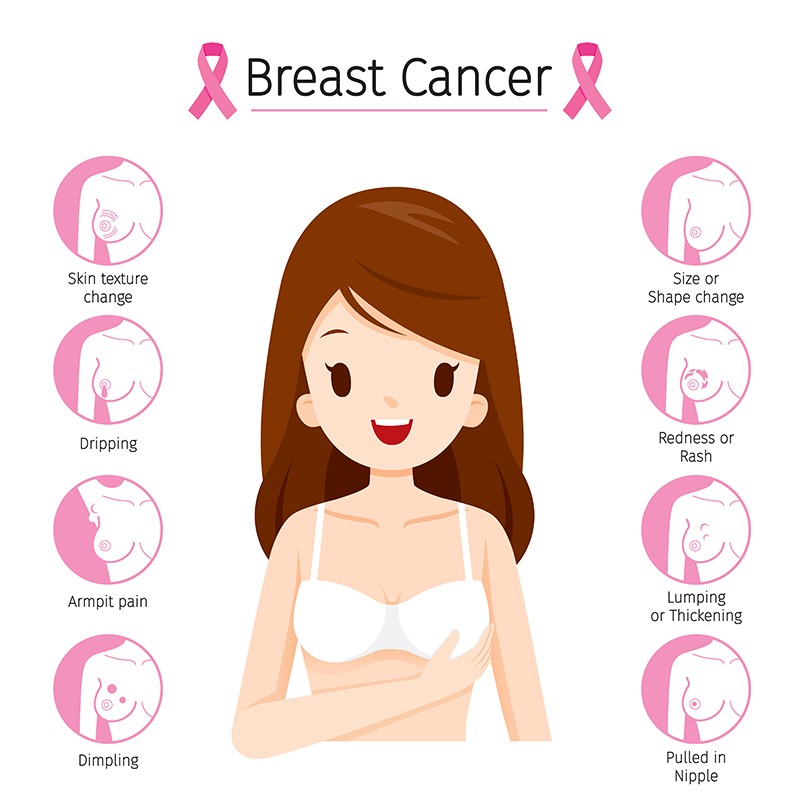
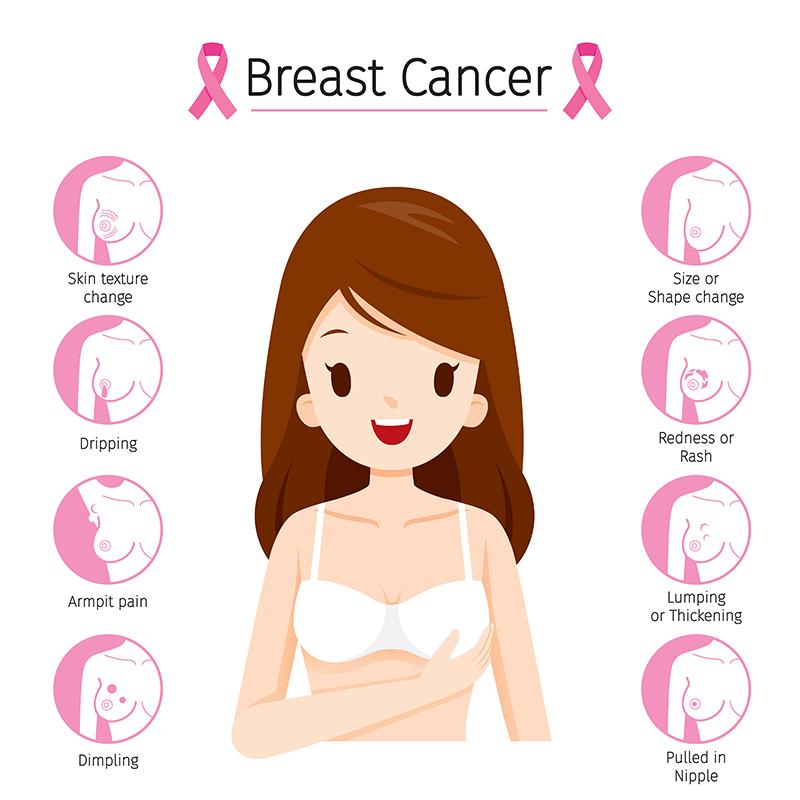
3. Symptoms.
At the early stage of the disease, the majority of women with breast cancer have no signs or symptoms that impact their health. Some women may fell “healthy” for months or even years while a tumour is already in their breast. In advanced stages, however, symptoms emerge.
![]()
Symptoms of breast cancer are highly variable and depend mainly on the location and extent of a tumour. In general, breast cancer symptoms may include:
- Weight loss.
- The Loss of appetite.
- Redness or retraction of the skin of the breast.
- The Yellowing of the “white of the eye (icterus).
- Change in the size or shape of the breast
- Inflammation and increased warmth in the breast
- Back pain, which may indicate bone metastasis
- Peeling or flaking of the nipple skin – sometimes accompanied by bloody discharge
- An irritating cough accompanied by shortness of breath – which may indicate lung metastases.
Note: If you experience these symptoms, it does not mean you have breast cancer; do not assume. Medical conditions other than cancer can cause these symptoms. Only your doctor can confirm your breast cancer diagnosis.
4. Diagnosis.
There are several methods of screening for breast cancer: breast self-examination (BSE), magnetic resonance imaging (MRI), ultrasound, estrogen and progesterone receptor tests, genetic testing, mammography every 1-2 years, and Biopsy.
- Breast self-examination (BSE) – a monthly breast self–exam is the easiest way to find breast cancer at an early stage. Women who practice regular self-breast examination have more chances to discover a smaller and less developed breast cancer than those who do not. They have more chance of being cured or live longer with the disease. You can start practising regular self-exam from the age of 20. By doing so, you will become familiar with the specific texture of your breasts and know to discover precancerous abnormalities or early cancerous growth at an earlier stage.
It is recommended to do a breast self-exam during non-hormonal stimulation, or seven to ten days after the end of your menstruation. If you are irregular or postmenopausal, you can choose a specific date to do the test; determine a time easy to be remembered and observed the following signs.
- Nipple discharge.
- The sensation of a lump or thickening of the breast
- The sensation of a nodule in the armpit or neck
- Localized retraction of the skin (like an orange peel) or the nipple.
- Persistent and painful inflammation of the skin of the breast.
- Eczema, redness or other abnormalities in the nipple/
- Visible or palpable change of breast.
Although you should always take seriously any recent change in the appearance of your mammary gland, a palpable nodule is not necessarily cancer. It may be another breast disease such as mastitis, cyst or fibroadenoma, the most common noncancerous breast tumour in young women. A change in your breast may merely be a hormonal change. Consult your doctor before you panic or assume anything.
- Clinical breast exam – your “self-breast exam” is not always enough to detect abnormalities in your beast; you may need a breast examination by your doctor. It is an important consideration; in fact, the American Cancer Society recommends this test once every three years until age 40 for even women who are not at risk. The monthly self-breast exam, clinical breast examination (by your doctor) and mammography are three critical tests in the early detection of breast cancer.
- Mammogram – this medical technique is performed in breast cancer diagnosis. It allows your physician to study your mammary gland and possibly detect anomalies, lesions and breast cancer even at an early stage. This examination is recommended to be performed when the breasts are not bigger due to menstrual cycle; the breasts are less sensitive to pressure from the mammogram and require lower doses of x-rays. The mammogram test is the most reliable in detecting breast cancer at a very early stage. In fact, early mammography can increase your chance of healing up to 90%.
Other tests such as clinical palpation, ultrasound, scintigraphy, CT scan, and magnetic resonance are often complementary to mammography and can in no way replace it. However, although the risk of developing breast cancer due to mammogram is negligible, excessive use can contribute to the development of breast cancer.
- Digital mammography (Senographe 2000D) – this screening method is a little bit recent but useful. Invented by General Electric, sonographer 2000D is approved by the FDA in January 2000 for the diagnosis of breast cancer. Digital mammography can detect breast cancer even when they are not palpable, but already manifest by fine calcifications or discrete changes in the anatomy of the breast. The image obtained with the Senographe 2000D is often more excellent than the standard imaging techniques.
- Computer–aided detection (CAD) – this radiological procedure is a recent advance in the diagnosis of breast cancer. It highlights microcalcification clusters and hyperdense structures in the soft tissue of the breast. However, CAD seems less useful in detecting early breast cancer than the digital mammography; therefore, it is often used complementary to a mammogram exam. Also, the CAD is more sensitive for microcalcifications than for masses.
- Scintigraphy – Scintigraphy is a medical technique consists of using radioactive materials to produce images of the breast.
This examination is particular in detecting malignancy, but it cannot detect lesions that are not larger than 1 cm. Scintigraphy presents no risk to your health because the injected fluid is quickly excreted in your urine. Scintigraphy is complementary a to a mammogram, and it is recommended:
- When the mammogram indicates the possibility of a malignancy.
- In cases of dense breasts that make difficult the interpretation of the mammogram.
- When the results of the needle biopsy are not sufficiently conclusive – showing little cancerous cells.
- In case the patient has had cosmetic surgery or breast implants.
- In case of complications of local cancer following a chemotherapy.
- If during the palpitation, your doctor has discovered a mass that is not visible on mammography – scintigraphy is used to determine if the mass is tumoral or not.
- Magnetic resonance imaging (MRI) Emerged in the early 1980s, MRI has become an essential tool in the diagnosis of many diseases including breast cancer. It is based on the principle of nuclear magnetic resonance (NMR) which allows your doctor to take a picture of the soft tissue of your breast. Unlike CT-scan, MRI is a noninvasive procedure that does not radiate. Also, it can visualise small sized-cancers through their neovascularisation. MRI participates widely in the diagnosis of tumours and their extension and plays an active role in many forms of biopsy. It is involved in treatment decisions, and sometimes even directly involved in the treatment. An MRI helps your doctor to monitor the evolution of cancer during and after treatment.
However, MRI can give false-positive results; therefore, it is often used in complementary to mammography.
- Breast ultrasound – a breast ultrasound is a medical procedure that allows your doctor to obtain images of your breasts by using sound waves of high frequency. Images captured give your doctor the possibility to evaluate abnormalities found during the mammogram or clinical exam. A breast ultrasound involves no radiation, poses no health problem.
- Biopsy – the imaging techniques can reveal a cancerous mass, but they can’t confirm the presence of cancer cells in your breast. Your physician will perform a biopsy to confirm the diagnosis accurately. In general, the biopsy consists of removing a sample from the breast tissue or cells where a tumour is suspected. The sample will be microscopically studied to obtain accurate information on the overall structure of the fragment removed. A biopsy is often associated with a bacteriological, immunological or biochemical study. There are different types of biopsy that your doctor can perform:
- Thin Needle aspiration biopsy(NAB) – also called fine needle aspiration cytology, NAB is a fast and straightforward procedure, yet reliable in detecting cancer cells. Usually, the pathologist uses a thin needle to extract tissue or fluid samples from the lump in the breast to examine under a microscope. The entire procedure can last 30 minutes or less.
- Large needle aspiration biopsy (LNAB) – this procedure is nearly the same as the fine needle aspiration cytology. The difference between the two is in the size of the needle.
- Surgical biopsy – performed under local or general anaesthesia, a surgical biopsy is the most reliable method to confirm a breast cancer accurately. The surgeon removes either a portion of a tumour (incisional biopsy) or an entire tumour plus the surrounding tissue (excisional biopsy) to allow a pathologist to do a microscopic examination. After analysis, your oncologist will be able to determine if your condition is cancer or a benign tumour.
- Stereotactic biopsy – this it is a painless removal of samples from a lump in your breast that is visible only by mammogram or ultrasound. During the procedure, your pathologist will use a particular computer to guide the needle to the lump from which he will take the samples. It is an outpatient procedure done under local anaesthesia, which can replace surgical biopsy with comparable reliability.
A certified technologist can perform a stereotactic, biopsy, but it requires interpretation by a physician or a board-certified radiologist.
5. Stages.
It is crucial for your doctor to determine if it has spread to other tissues or organs of your body such as the lymph nodes in the armpit.
Staging tests – your doctor can base on the same exams performed in the diagnosis to determine the stage of cancer. In some cases, however, additional tests are needed. Your doctor may remove several lymph nodes for microscopic analysis. After removal, the sample will be sent to a pathologist for microscopic examination to look for signs indicating metastases; in case the test is positive, you are diagnosed with metastatic breast cancer.
Knowing the stage of your breast cancer is very important for your oncologist to determine the type of treatment you must undergo. Your doctor will base on the stage of the breast cancer to recommend the procedure most appropriate and capable of combatting the disease. In general, breast cancer stages include the following:
- Breast cancer in situ – this stage of breast cancer is commonly known as stage 0 breast cancer; it represents 20% or less of breast cancers. There are two types of breast carcinoma in situ.
- Lobular carcinoma in situ(LCIS) – LCIS is often detected during a mammogram.
- At this stage, the tumour is not considered cancerous; the scientists call it carcinoma in situ or stage 0 breast cancer. However, it is taken into consideration, for those who have lobular carcinoma have up to 25% chance of developing breast cancer in the next 25 years.
- Ductal carcinoma in situ (DCIS) – also called intraductal carcinoma, DCIS is a particular form of breast cancer, a very early stage that has not spread beyond the lobule. During this stage, there is no infiltration of cancer cells through the fatty breast tissue or the membranes surrounding the lactiferous. Intraductal carcinoma accounts for nearly 25% of all breast cancer diagnosis. As lobular carcinoma in situ, ductal carcinoma in situ is often detected during a mammogram.
- Stage I – in this early stage, the size of a breast tumour is usually 2 centimetres or less, and the breast cancer has not spread outside. If you are diagnosed with a stage 1 breast cancer, you are more likely to be cured.
- Stage II – a stage 2 breast cancer can present in three different characteristics:
- Stage IIA breast cancer – the size of a breast tumour remains less than or equal to 2 centimetres but has spread to axillary lymph nodes in the armpits.
- Stage IIB breast cancer has a size between 2 and 5 cm with or without having spread to lymph nodes in the armpit.
- Stage IIC – the size of cancer is more than 5 cm, but it has not spread to lymph nodes in the armpit.
- Stage III – the specialists in ecology divide stage III breast cancer in three substages (categories): stage IIIA, IIIB and IIIC.
- Stage IIIA breast cancer – during stage IIIA, 1) the extension of cancer is less than 5 centimetres and has spread to axillary lymph nodes and the lymph nodes are connected with each other or with other structures. 2) The size of the cancer is higher than 5 centimetres and has spread to axillary lymph nodes.
- Stage IIIB breast cancer – during stage IIIB, on the other hand, 1) cancer has spread to nearby tissues of the breast (chest wall, ribs, chest muscles). 2) The breast cancer has spread to lymph nodes inside the chest wall. At this stage, your survival chances decrease.
- Stage IIIC breast cancer can be of any size and has spread to. 1) 10 or more lymph nodes under the arm; 2) lymph nodes above or beneath the collarbone and near the neck; 3) lymph nodes under the arm.
- Stage IV: this final stage indicates very advanced breast cancer. Cancer has metastasised to other organs of the body such as bones, lungs, brain. A tumour may be extended locally to the skin and internal lymph nodes in the neck.
- Recurrence – breast cancer is considered as recurrent when it returns after treatment. Cancer can develop in the original location or other sites. In general, recurrent breast cancer is more difficult to eradicate; survival chances decrease considerably.
6. Treatment.
Breast cancer treatment varies depending on the stage or the severity of a tumour at diagnosis. In fact, not only the treatment, even the prognosis depends somehow on the BCSAD (breast cancer stage at diagnosis). Mostly, five types of treatment are used to fight breast cancer: chemotherapy, radiotherapy, hormone therapy, biological therapy and surgery.
-
Chemotherapy
Chemotherapy is a systemic cancer treatment consists of using strong drugs to shrink or eliminate a tumour in your breast. The drugs travel your body through the bloodstream to destroy cancer cells. For some breast cancers, chemotherapy is beneficial and can progress to a cure.
However, in addition to cancer cells, healthy cells are also damaged by the chemotherapy, which leads to side effects such as:
- Hair loss.
- Weight loss.
- Decreased appetite.
- Darkened and thickened skin.
- Blistering skin or acne.
- Mouth blistering.
- Dry mouth.
- Fatigue.
- Painful urination or red urine.
- Black, tarry stools.
- Unusual bruising or bleeding.
- A cough.
- Congestion.
- Fever.
- Dizziness.
- Chills.
- Shortness of breath.
- A sore throat.
- Swelling of the feet or ankles.
- Nausea and vomiting.
- Skin rash.
Chemotherapy drugs can be taken by mouth, intravenously or intramuscularly. At first, chemotherapy drugs approved for the adjuvant treatment of breast cancer was a combination of cyclophosphamide (Cytoxan), methotrexate (Trexall, Rheumatrex) and 5-fluorouracil (5-FU). In recent years, however, other drugs are added up in the treatment of breast cancer.
Among which, there are Adriamycin (doxorubicin) and Taxol (paclitaxel); they seem to bring good results in the fight against breast cancer.
-
Radiation therapy (Radiotherapy)
Radiation therapy is a medical procedure involving the use of x-rays at high energy to kill cancer cells and shrink a tumour. Unlike chemotherapy, which is systematic, radiotherapy delivers a precise dose of radiation to the volume of a tumour, thus, sparing the maximum surrounding healthy tissue possible.
Choosing the exact dose (amount of energy that radiation will deposit in the tissues) of radiotherapy is very important. According to many recent studies, underdosing beyond 5% is less effective and increases the risk of recurrence. Therefore, your oncologist will recommend the dose the most capable of fighting cancer.
Usually, you are administered the therapy 4 or 5 days per week for a period of 5 to 6 weeks consecutively. A session of radiation can last 20 minutes or less. The treatment is painless (does not cause pain), but cause side effects, which may include:
- Fatigue
- Discolouration of the breast.
- Red Lips.
- Constipation.
- Vomiting and nausea.
A healthy and well-balanced diet and medicines can be used to Remedy those effects.
During and after the therapies (chemotherapy and radiotherapy), medical surveillance is essential.
Some complications especially heart, lung and digestive problems; arm swelling may occur several years after the radiotherapy and chemotherapy. However, with the invention of sophisticated and computerised machines, radiation has become less dangerous and causes less or no side effects. If your doctor thinks it will be helpful, he will recommend internal radiotherapy (brachytherapy) along with the external radiation therapy.
-
Brachytherapy
Also called internal radiotherapy, sealed source radiotherapy or curietherapy, brachytherapy is a type of radiotherapy consists of introducing the radioactive sources inside the breast next or directly in a tumour. Brachytherapy is based on the same principle as radiotherapy; the difference is that radioactive sources are introduced directly into cancer, which makes this method less destructive to healthy surrounding cells of the treated area.
Also, brachytherapy can only be performed to treat non-metastatic cancers. Two main types of brachytherapy can be used in the treatment of breast cancer:
- Interstitial: during interstitial brachytherapy, your oncologist will place the radioactive source directly into your breast. The radioactive material can be in the form of plastic tubes, hollow metal needles, seeds or wires. In general, these materials are placed under the skin of your breast after receiving local, epidural or general anaesthesia.
- Endocavitary: this form of radiotherapy consists of placing the radioactive source in natural cavities of the breast affected by cancer. Endocavitary irradiation therapy allows your doctor to irradiate a tumour while protecting surrounding organs.
Note: Endocavitary irradiation therapy is in an experimental phase and not yet approved by the FDA.
-
Hormone therapy.
In some types of cancers such as breast cancer and prostate cancer, the cancer cells depend on hormones to multiply; these types of cancers are called hormone-dependent cancers. Therefore, to stop the proliferation of the cancerous cells, your doctor may recommend you take drugs capable of blocking hormonal stimulation. Along with chemotherapy or radiotherapy, hormone therapy (HT) is commonly used to fight breast cancer; results vary from one patient to another. In general, hormone therapy is less toxic and causes fewer side effects than chemotherapy.
However, this therapy cannot be used in all types of breast cancer. Some young and pre-menopause women sometimes have tumours that are not hormone receptors; the cancer cells are not sensitive to hormone therapy.
In the treatment of breast cancer, hormone therapy may include two groups of drugs: selective estrogen receptor modulators (SERMs) and aromatase inhibitors.
Selective estrogen receptor modulators (SERMs): this class of drugs acts by blocking the action of estrogen in breast tissue, thus preventing breast cancer cells to multiply. These drugs act like estrogen on some cells (by stimulating the estrogen receptors) while blocking the effects of estrogen on other cells (by inhibiting the estrogen receptor). SERM has a preventive and curative effect against breast cancer; it kills cancer cells and reverses the growth of a tumour.
Tamoxifen is one of the SERM which has revolutionised the hormonal treatment of breast cancer. It can be used in the prevention and treatment of breast cancer. Raloxifene is another SERM drug group and has characteristics similar to tamoxifen. However, it has a half-life much shorter than tamoxifen and should be used in a higher dose.
Side effects of selective estrogen receptor modulators may include:
- Night Sweats
- Water retention
- Weight loss
- Irregular menstrual periods
- Hot flashes
- Vaginal itching, discharge or dryness.
Older women may experience severe complications such as:
- Bone pain.
- Back pain.
- Headaches.
- Coughing.
- High cholesterol.
- Blood clots.
- Endometrial cancer.
Aromatase inhibitors: aromatase inhibitors are a recent class of drugs used in hormone therapy to treat breast cancer in menopausal women. They act by reducing estrogen levels in the blood of postmenopausal women.
They inhibit or inactivate aromatase, an enzyme responsible for the synthesis of estrogens from androgens of adrenal origin. Unlike tamoxifen, users of aromatase inhibitors may experience one adverse effect, increased risk of osteoporosis; they generally are well tolerated by most women. The most common aromatase inhibitors are anastrozole (Arimidex), letrozole (Femara) and exemestane (Aromasin).
-
Surgical treatment
Although surgery can lead to pain and other adverse effects, if you have breast cancer, your chance of undergoing surgery to remove a tumour is very high. The type of surgery performed depends significantly on the size of a tumour. Your surgeon may, at the same time, conduct an axillary lymph node dissection on the same side as a tumour to determine if cancer has spread to the lymph nodes. In general, the surgeon will perform one of the following surgical procedures:
Lumpectomy: often performed in the surgical treatment of breast cancer, lumpectomy is a surgical procedure consists of removing breast tumour (benign or cancerous) and tissue that surrounds it. Usually followed by radiotherapy to kill cancerous cells remaining in the breast tissue. Your surgeon may also remove some axillary lymph nodes during the lumpectomy. However, some tumours cannot be eradicated by lumpectomy:
- a large cyst.
- cancer deep within the breast.
- cancer metastasis (in the same breast).
- Inflammatory breast cancer.
- Also, if you have already had radiation therapy or suffer from a connective tissue disease, a lumpectomy may not be appropriate for you.
Partial mastectomy – also called segmental mastectomy, a partial mastectomy involves the surgical removal of a tumour along with a significant amount of breast tissue and some skin. Depending on the extension of a tumour, your surgeon may also remove a small part of your chest and some lymph nodes. As for lumpectomy, partial mastectomy is often followed by radiation therapy.
Simple mastectomy – this surgery is more radical than both lumpectomy and partial mastectomy; it involves complete removal of the breast: nipple, areola, lobules, ducts, fatty tissue and skin. A mastectomy may be followed by radiation therapy, chemotherapy or hormone therapy. After surgery, the surgeon may recommend you breast prosthesis until a date when it is possible to consider reconstruction.
Modified radical mastectomy: This method is the most performed surgical intervention in the treatment of breast cancer. It involves the removal of the entire breast including the nipple and the skin tissue but without removing the pectoral muscles, which includes pectoralis major muscle and pectoralis minor muscle. Your surgeon may remove some axillary lymph nodes to determine if cancer has metastasised.
Radical mastectomy: this is total removal of the breast including underlying pectoral muscles and axillary lymph nodes. Your surgeon will perform this operation if the cancer is deep within your breast or if the cancer cells have invaded your chest wall.
Reconstructive surgery – If you have a mastectomy, it can negatively change your appearance, and causes emotional and social impacts on you. You do need a breast reconstruction to help you overcome those problems.
However, this could be done at the time of the mastectomy or later after the surgery. Breast reconstruction may include reconstruction of your nipple and areola, reconstruction with implants, rebuilding with a tissue flap, or deep inferior epigastric perforator (DIEP) reconstruction. However, not all women can have these operations; talk to your doctor for more details.
-
Biological Therapy
Cancer and its treatment often weaken the immune system. Biological therapy, also called biotherapy or immunotherapy, is the use of natural or synthetic substances to stimulate and strengthen the immune system. This therapy can be used to fight cancer or reversing the side effects caused by the treatment. The most commonly used drugs in immunotherapy include:
Trastuzumab (Herceptin) – This medication is sometimes very useful in fighting breast cancer. It is a monoclonal antibody that reacts against HER2 (Human Epidermal growth factor Receptor 2)-Neu, a protein of which level is aggressively higher in approximately 20% of patients treated for breast cancer.
Along with chemotherapy, Herceptin can shrink or eliminate a tumour. Trastuzumab is approved by the FDA (Food and Drug Administration) for the treatment of breast cancer.
Bevacizumab (Avastin) – Avastin is a humanised monoclonal antibody that works by binding to VEGF (vascular endothelial growth factor) and inhibits its binding to its receptor Flt-1 (VEGFR-1) and KDR (VEGFR-2), two chemicals located at the surface of endothelial cells that contribute in the growth of new blood vessels.
In a simple term, Avastin inhibits the formation of new blood vessels and prevents them from growing. Moreover, they end up dying. Avastin is also approved by the U.S. Food and Drug Administration (FDA) in the biological therapy of breast cancer.
Lapatinib (Tykerb) – in 2007, this drug was approved by the US Food and Drug Administration (FDA)for the treatment of patients with advanced or metastatic breast cancer whose tumours overexpress HER2, and who have received prior therapy including an anthracycline, taxane, and Herceptin
7. Preventions.
If being cured or recovered from breast cancer is hypothetic, its prevention is somehow different. Some preventive methods can help you reduce breast cancer risks in the short and long term.
 Taking the following steps can help you not only reduce the risk of developing breast cancer but also its reoccurrence if you already diagnosed with it:
Taking the following steps can help you not only reduce the risk of developing breast cancer but also its reoccurrence if you already diagnosed with it:
- Chemoprevention
This method consists of using natural or synthetic substances to prevent, reverse, or delay the development of cancer cells. Micronutrients such as iron, cobalt, chromium, copper, iodine, manganese, selenium, zinc and molybdenum, as well as other nutrients like calcium, and folic acid (Vitamin B9) are often used.
Other medications used in chemoprevention of breast cancer in women at low or average risk for breast cancer include tamoxifen or raloxifene (Evista). When it comes to your health, prevention is always better than treatment, which does not always lead to cure; make your first step today to prevent breast cancer.
- Lifestyle
Your lifestyle plays a crucial role in preventing breast cancer or your survival chances if you are already diagnosed with the disease. In fact, some women have breast cancer due to their unhealthy lifestyle.
You can reduce your chance of having breast cancer by practising the following preventive methods:
Avoid Hormone therapy for menopause symptoms – although menopause is not a disease, its symptoms can be troublesome in some women. To relieve these symptoms, some women use menopause hormone therapy (MHT). While it can be helpful, some hormonal treatments can cause serious health problems; in fact, long-term use of menopausal hormone therapy (MHT) may lead to breast cancer. According to the World Health Organization (WHO), MHT is a risk factor for breast cancer especially when taken for more than five years.
Practice Prolonged Breastfeeding – it may sound old fashion, but prolonged breastfeeding is right for you and your child. Studies have shown that the practice helps reduce the risk of breast cancer occurrence, and provides many benefits in the physical and mental development of the infant. In another word, by breastfeeding you increase the chance of your infant to be healthy, and decrease your risk of developing breast cancer.
Avoid contraceptive containing estrogen: Some cancer cells (breast cancer cells for instance) need sex hormones to survive. Some studies have shown an increased risk of breast cancer in women taking oral birth controls containing synthetic estrogen. Although controversial, it is wise to use oral contraceptives medications that do not contain synthetic estrogen hormones.
Maintain a healthy weight – being overweight increases the risk of a variety of disease, including breast cancer. The risk is even higher in post-menopausal women and women with high levels of estrogen (hormone). It is estimated that a global reduction of obesity could prevent more than 10,000 new cases of breast cancer per year. Therefore, if you do want to prevent breast cancer; you need to maintain a healthy weight.
Regular physical exercise – there is no benefit in being physically inactive; the wages of physical inactivity is disease and death, not less than the “wages of sin is death”. Practising 30-45 minutes of exercise daily, at least four days a week can reduce the risk of breast cancer by up to 40%.
Not only exercise can prevent the formation of new cancer cells, but it can also kill cancer cells in their genesis. Whether you have breast cancer, at risk or feel concerned, regular exercise is beneficial for you.
Avoid alcohol and tobacco use – the risk of breast cancer is higher with consumption of alcohol and smoking of a cigarette. Even moderate consumption of alcohol and second-hand smoking can increase the risk of breast cancer 20% to 30%. In addition to breast cancer, tobacco is the number one cause of oral and lung cancers.
- Preventive surgery
Although it is not appreciated by the majority of people living with cancer or women at high risk, an operation is often performed as treatment or/and prevention of breast cancer. If you are at high risk of breast cancer, your doctor can lower your risk by implementing a preventive breast removal.
In some case, precautionary removal of your ovaries can be done if you have increased chances of developing ovarian cancer. In general, your oncologist may consider one or both of these surgeries to reduce your risk of developing breast cancer or/and ovarian cancer:
Mastectomy: this surgical procedure is one of the most effective methods to prevent breast cancer. Mastectomy involves removing one or both breasts, surrounding tissue that is considered as pre-cancerous.
Although radical, this technique saves the lives of thousands of high-risk women for breast cancer.
Prophylactic oophorectomy: this is another type of surgery your doctor may consider to reduce your risk of breast cancer and ovarian cancer. This preventive method can reduce up to 95% risk of ovarian cancer and 60% of breast cancer if it is performed before the age of 35. Prophylactic oophorectomy involves the removal of both ovaries.
In general, it is performed for women with a high risk of breast cancer and ovarian cancer due to an inherited mutation in their BRCA1 or BRCA2 gene.
8. Prognosis.
Despite billions of dollars spent on research, cancer continues to make speak of it as being the second primary cause of death in the U.S. Each year; the disease causes the death of about 559,888 people.
Breast cancer alone kills around 41.528 women each year in the United States; this represents an estimate of 4 deaths per hour. With nearly 205.000 new cases each year worldwide, breast cancer becomes a matter of concern for all women in the world.
However, there is hope that the breast cancer survival rate will steadily increase.
Over 80% of women who have breast cancer live more than ten years. This rate, nevertheless, varies by race; from 1999-2005, the overall 5-year survival rate was 89.1%, with 90.3% for white women and 77.9% for black women.
Although minimal, some victims completely recover from the disease; do your best to be one of them. However, your chance of being cured or surviving for over ten years depends on various factors:
Location and extension of a tumour – You’re less likely to survive if cancer has spread into your lymph nodes or other organs in your body. The risk of recurrence increases compatibly with the number of axillary lymph nodes affected. Thus, with more than ten cancerous lymph nodes, you have a great chance to see the disease return after treatment. The size of the lymph node affected by the cancer is also significant.
Size of a tumour – the size of a breast tumour plays a significant role in your survival chance. Large breast cancer tends to spread or metastasise to other organs in your body; thus:
- A tumour smaller than 1 cm, the five–year survival rate is approximately 90%
- A tumour of 1 to 2 cm, the five–year survival rate is around 75%.
- A tumour of 2cm to 5cm, the five–year survival rate is 30% to 40%.
- A tumour 5 cm or more, the five–year survival rate is less than 25%.
Invasion of a tumour – you can be diagnosed with noninvasive breast cancer or invasive breast cancer:
Noninvasive breast cancer: If you are lucky to detect a tumour in its early stage, your chance of being completely cured is very high. For carcinoma in situ that is localised and has not reached the lobules, the likelihood of recurrence is very low.
- Invasive breast cancer: invasive cancer that has spread locally or into other organs, the chance of survival depends on the size of a tumour and the type of organs it has invaded. Usually, a tumour that has spread into the lymphatic system of the breast is less dangerous; in the other hand, cancer that has affected the muscles of the chest may present serious complications. The survival chance considerably decreases.
Hormone-receptor-positive or contrary– You have a higher chance to survive if your tumour is hormone receptor positive. Your breast may contain hormone receptor-positive cells or hormone receptor negative cells.
Hormone receptor-positive cells do not grow much, but they produce large quantities of receptors for estrogen and progesterone. Hormone receptor negative cells, on the other hand, produce fewer hormone receptors, but they have more potential for growth.
If the hormone receptor-negative cells are healthy, they turn into hormone receptor-positive cells and have their characteristics. When they are cancerous, these cells remain in a state of hormone receptor negative and multiply anarchically. Therefore, you have a better chance of survival if your tumour is receptor-positive.
Genetic – there are at least three genetic factors that may contribute to your prognosis:
- No diploid DNA – the healthy breast cells are diploid (chromosomes it contains are present in pairs) and have the ability to produce two copies of each chromosome. Cancer cells, on the other hand, do not respect this reproduction. This lack of diploid cell makes the risk of breast cancer recurrence nearly three times higher.
- High level of cell reproduction – cell division is the mode of multiplication of any cell. When the division is healthy, it allows a cell to divide into two daughter cells; one cell becomes two, and then four, then eight and so on. Cancer cells, however, divide like crazy; this abnormal cell division is the characteristic of cancer cells.
- Presence of certain neu-oncogenes – overexpression of specific genes such as HER-2/neu (Human Epidermal Growth Factor Receptor-2) tends to amplify the aggressiveness of breast cancer in up to 30% of breast cancer patients. If you have this condition, you have an increased risk of recurrence and worse prognosis.
Note: Although fighting cancer is very stressful, a happy mood and healthy lifestyle during and after the treatment have a substantial impact on your survival chance. Be comfortable and confident during and after the therapies.