Table of Contents
Vaginal cancer refers to formation of malignant growth (cancer) in the tissues of the vagina. Although vaginal cancer occurs in very young women, the cancer affects mainly elderly women. In fact, almost 75% of vaginal cancer patients are aged over 60 years. There are also cases of cancer of vagina in very young girls, of whom mothers have received hormone therapy – specifically estrogen – during pregnancy.
While the majority of Primary vaginal cancers occur on the posterior vagina, the tumor tends to spread either by direct extension into adjacent organs (rectum, bladder, etc), or through the bloodstream to invade the lymph nodes in the groin or other remote sites. Therefore, you have a better chance of surviving when you are diagnosed with early-stage vaginal cancer.
Types of Vaginal Cancer
Depending on the group of cells affected, a vaginal cancer can be:
Squamous cell vaginal cancer (or Vaginal squamous cell carcinoma)– this type of vaginal cancer is the most common; it arises from the thin, flat squamous cells that line the vagina. Squamous cell vaginal cancer represents 75 to 90% of malignant tumors of the vagina. Vaginal squamous cell carcinoma spreads slowly and usually develops in women aged 60 or older.
Adenocarcinoma vaginal cancer (or vaginaladenocarcinoma) -this type of vaginal cancer is rare, representing 5 to 10% of malignant tumors of the vagina. Usually, the cancer arises from the cells in the lining of the vagina that produce vaginal mucus. Unlike squamous cell vaginal cancer, vaginal adenocarcinoma is more common in young women.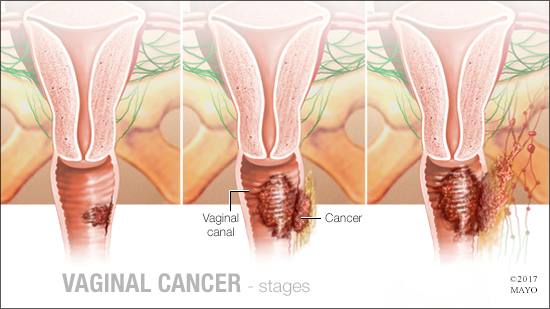
Vaginal melanoma – this is a very rare form of vaginal cancer. Usually, vaginal melanoma arises from “the pigment-producing cells in the vagina. It is responsible for 1 to 3% of cancers of the vagina. Vaginal melanoma tends to occur among older women, mostly women aged 60 or older.
Vaginal Sarcoma – Sarcomas are very rare. They usually begin in the connective tissue cells or smooth muscle cells in the walls of the vagina. Unlike vaginal squamous cell carcinoma, vaginal sarcomas tend togrow fast, and lead to complications. There are at least three types of vaginal sarcomas:
- Leiomyosarcoma –this malignant tumor develops in the involuntary muscle cells of the vaginal walls; it is the most common type of vaginal sarcomas. Usually, leiomyosarcoma is found in women aged 50 or older.
- Rhabdomyosarcoma –this subtype of vaginal cancer arises from the voluntary muscle cells of the vaginal walls. Unlike leiomyosarcoma, habdomyosarcoma occurs mostly in girls aged 3 or younger.
- Embryonal rhabdomyosarcoma– also called sarcoma botryoides, embryonal rhabdomyosarcoma is a rare but aggressive form of vaginal sarcoma. It is often found in children less than 8 years of age. Although the tumor arises from cells of the vaginal walls, with times, it can show outside the vagina, and cause severe pain.
Vaginal Cancer Incidence
Primary vaginal cancer (the cancer begins in the vaginal tissue) is a rare tumor, representing 1 to 3% of cancers of the female genital tract. Worldwide, the incidence of primary vaginal cancer is estimated at 0.3 to 1 / 100 000. Vaginal cancer is responsible for 1% of gynecologic cancers in the U.S., with nearly 2.400 women diagnosed with the disease each year. According to the National Cancer Institute (NCI), it is estimated that there were approximately 2.160 women diagnosed with vaginal cancer in the United States in 2009; about 770 women died of the disease.
Vaginal Cancer Causes
The vagina should not be confused with the vulva, all external parts of the women reproductive tract. The vagina is the organ through which a woman has sex, evacuates fluids during menstruation and gives birth. It is a muscular and very elastic duct, about 12 cm in length, which extends from the uterus to the vulva. The interior of the vagina is covered with a thin mucous membrane (vaginal mucosa) that has many transverse ridges (vaginal rugae) as well as many nerves allowing it to have certain sensitivity. The vaginal mucosa constantly produces various secretions to keep the vagina more or less humid.
Vaginal cancer occurs when certain cells lining the vagina multiply anarchically t form a malignant growth. These cells never stop to grow, and leading to formation of cancerous lesions in the vaginal cavity. In other words, vagina cancer is characterized by uncontrolled proliferation of abnormal cells that line the inner surface of the vagina.
Vaginal Cancer Risk Factors
Many factors are suspected in the development of vaginal cancer; the most common include:
- smoking
- multiple sexual partners (the fact that it increases your risk of STDs)
- history of cervical cancer
- having had a hysterectomy
- having had radiation therapy to the pelvic area
- Age – squamous cell vaginal canceris more common in women aged 50 or over
- history of human papillomavirus (HPV) disease such as genital warts
- certain precancerous conditions in vagina such as vaginal intraepithelial neoplasia (VAIN)
- having taken diethylstilbestrol (DES) during pregnancy
- Personal history of gynecologic cancer, especially cervical cancer.
Vaginal Cancer Symptoms
In early development of the disease, vaginal cancer can be completely asymptomatic; the tumor is growing in your vagina without producing any symptoms. When symptoms finally emerge, vaginal cancer is characterized by abnormal vaginal bleeding that sometimes occurs after intercourse. The bleeding may be intermenstrual (occurs between menstrual periods) or postmenopausal (after menopause). In addition to non-menstrual bleeding, you can experience the following conditions:

- difficult or painful urination
- vaginal pain during intercourse
- pain in the pelvic area
- Presence of lump or mass in your vagina
- Constipation
- Watery vaginal discharge which is often bloody and foul smelling.
Vaginal Cancer Complications
Vaginal cancer is sometimes subject to metastases. The cancer can invade paravaginal local tissues such as the bladder or rectum. In addition, the tumor can affect pelvic organs such as the pelvic bones through the inguinal lymph nodes or through the pelvic lymph nodes. Advanced vaginal cancer can spread into other distant sites of the body such as lungs and liver through the bloodstream.
Vaginal Cancer Diagnosis
Even if you have the symptoms above, you should not conclude you have vaginal cancer. A Vaginal cancer diagnosis must be done and confirmed by a medical professional. Therefore, if you experience symptoms of vaginal cancer, it is important that you see your gynecologist immediately. The earlier the cancer is diagnosed and treated, the higher is your chance of surviving.
The following diagnostic procedures are often performed in vaginal cancer diagnosis:
Pelvic Exam – your doctor will do an internal vaginal examination to examine not only your vagina but also other organs of your pelvis to search for signs indicating a vaginal cancer. A speculum examination allows your physician to identify a tumor sometimes in its genesis or more often a bleeding ulcer, which may indicate the cancer.
Pap smear (Pap test) – a Pap smear is a simple and painless medical procedure allowing your physician to check for changes in the cells of your cervix. During the exam, your doctor will collect sample of cells from the cervix to be analyzed under microscope to search for precancerous transformation (dysplastic cells). This is a screening test rather than a diagnosis; the diagnosis is done through a biopsy.
Vaginal biopsy – this histological exam is usually performed under local anesthesia. During the procedure, the specialist collects sample of mucosa from the vagina by a pinch biopsy instrument for histopathological examination. This biopsy is recommended if your doctor finds suspicious vulvar lesion during the pelvic exam. Vaginal biopsy is especially necessary among older women in whom vaginal cancer is more common.
Colposcopy – this is an important examination in vaginal cancer diagnosis; it allows your doctor to examine your vagina using a binocular microscope (colposcope) that grows twenty to fifty times more the surface of your vagina. A colposcopy allows your physician to detect abnormalities in the vagina: precancerous lesions, cancerous growth, HPV infection, etc.
CT scan – this is an imaging technique that allows detection and visualization of abnormalities in the vagina by submitting the pelvic area to an x-ray beam. This technique is very important in the diagnosis of vaginal cancer; it gives precise images; thereby your doctor can detect whether the cancer is metastatic or not. However, repeated CT scan can be harmful to your body.
Magnetic resonance imaging (MRI) – with an MRI, your doctor can visualize organs inside of your body. In the case of vaginal cancer diagnosis, he can analyze the structure of your pelvis to look for abnormalities and highlight presence of a malignant mass. MRI not only allows your physician to detect the cancer but also to know the exact size and extent of the tumor.
Vaginal Cancer Stages
Once the cancer is detected in your vagina, it is necessary that your doctor knows its stage so that he can determine the most appropriate treatment to combat it. In addition, knowing the stage of the cancer gives your doctor an idea of the prognosis.
Vaginal cancer includes the following stages:
- Carcinoma in situ – also called stage 0, carcinoma in situ indicates the genesis of the cancer cells on the first layer of the vaginal wall.
- Stage I – the cancer is confined to the vaginal wall.
- Stage II – the cancer may have spread to paravaginal tissue, but has not spread into the pelvic wall.
- Stage III – the cancer has spread to the pelvic wall: nearby lymph nodes or the pelvic wall, or both.
- Stage IV A – the cancer has spread to distant sites of the vagina or rectum, bladder or pelvis.
- Stage IVB – the cancer has metastasized into distant sites such as the lungs.
Vaginal Cancer Treatment
To determine the most appropriate treatment, your doctor will base on the location of the tumor in your vagina and its stage. Overall, vaginal cancer treatment typically involves surgery, radiation therapy and sometimes chemotherapy.
Surgical Treatment
There are several types of surgery that your surgeon can perform. Surgery performed depends on your age, your health in general, the location and stage of the cancer. In general, surgeries that can be performed in vaginal cancer treatment include:
- Laser Surgery – this surgical intervention is reserved for cancers limited to the surface of the vagina. During the procedure, your surgeon will use a narrow beam of light to destroy the cancer cells in the vagina.
- Wide local excision (WLE) – WLE is a surgical procedure performed to remove the tumor and surrounding healthy tissue. In most cases, after the surgery, the surgeon takes pieces of skin or flaps of muscle from other areas of your body to repair your vagina.
- Vaginectomy – this is a surgical removal of part or the entire vagina. In general, vaginectomy is performed in cases of invasive vaginal cancer. During the surgical intervention, your surgeon can also remove the lymph nodes (lymphadenectomy) nearby. In certain cases, the vaginectomy may be accompanied by a hysterectomy, removal of the uterus, ovaries and fallopian tubes. Vaginectomy is often followed by brachytherapy and chemotherapy.
- Pelvic exenteration (or pelvic evisceration) – other surgical intervention above may not be suitable for recurrent vaginal cancer or cancer that has spread throughout your pelvic area. In this case, your surgeon will perform a pelvic exenteration to remove your lower colon, bladder, ovaries, uterus, vagina, and rectum. After which, your surgeon will make a urostomy to allow urination, and colostomy to allow feces leave your body.
Radiation Therapy (Radiotherapy)
If you have a stage II, III or IV vaginal cancer, the surgery must be followed by radiation therapy to destroy locally the remaining cancerous cells and reduce the risk of recurrence or metastasis. In rare cases, however, radiotherapy can be administered before surgery in order to reduce the size of the tumor to facilitate its excision.
- External beam radiation therapy – this method involves projecting high-dose of X-rays to the tumor to eliminate or shrink it. External radiation therapy is usually administered on an outpatient basis, five days a week for several weeks.
- Internal Radiotherapy – during this procedure, small tube containing radioactive material are inserted into your vagina for several hours to several days. Unlike external radiation therapy, internal radiation therapy requires hospital stay.
Chemotherapy
Chemotherapy can be included in the treatment. In general, you will be given powerful chemicals to stop or slow reproduction of cancer cells. You will be recommended chemotherapy if you have a very aggressive vaginal cancer: a cancer that spreads very quickly, or has spread beyond the vagina. In the treatment of vaginal cancer, chemotherapy drugs are usually taken intravenously.
However, the chemotherapy drugs attack both the cancer cells and healthy cells, which often cause side effects. Side effects vary from one person to another, from one drug to another. Most common side effects of chemotherapy include:
- nausea
- low blood cells count
- stomach pain
- vomiting
- loss of appetite
- temporary hair loss
- increased vulnerability to infections
- fatigue
Vaginal Cancer Prognosis
Prognosis of vaginal cancer depends on the stage of the cancer at diagnosis, your age and state of health to endure the treatment. In general, you’re more likely to survive when the cancer is detected early.
The 5-year survival of vaginal cancer is approximately:
- 65 to 70% at stage I
- 45% at stage II
- 30% at stage III
- 15 to 20% at stage IV.
Vaginal Cancer Prevention
Routine gynecological exam is the best way to detect any change or precancerous lesions in your vagina. This preventive measure can help your doctor to detect and remove precancerous abnormalities in your vagina. Routine pelvic exam also allows your gynecologist to detect cancer in its genesis which will benefit non aggressive but effective treatment.
Early diagnosis and adequate treatment of HPV infections are also important. The onset of clinical signs such as vaginal discharge, irregular bleeding, and pelvic pain should not be neglected. In addition, urinary or rectal abnormalities should not be overlooked. Report these changes to your physician so that he can perform an exploratory clinical and gynecological exam.
There are other factors that may lead to the development of vaginal cancer that deserve your attention. To reduce your risk of vaginal cancer and many other cancers, you need to:
- Stop smoking – cigarette smoke – including second hand smoke – increase the risk of all types of cancer including vaginal cancer. Therefore, if you really are serious to reduce your risk of having cancer, cigarette should be your enemy.
- Adopt healthy diet – there is an increased risk of vaginal cancer linked with the consumption of saturated fat, especially animal fats and fried foods. In the other hand, a regular consumption of fruits, vegetables and cereals (especially high in beta-carotene) reduce the risk of vaginal cancer and many other cancers.
- Exercise regularly – many studies have shown that physical activity reduces the risk of several types of cancer including vaginal cancer after menopause. In addition, regular exercise can boost your confidence and improve your self-esteem.
- Maintain a healthy weight – being overweight can play a role in the development of all cancers. A Dutch epidemiological research that followed 25 000 women aged 40 to 65 years over a period of 13 years found that overweight was among postmenopausal women one of the two main risk factors for gynecological cancers.
- Limit your alcohol intake – moderate drinking poses no risk of cancer, heavy alcohol consumption, in the other hand, is a causative factor.