Table of Contents
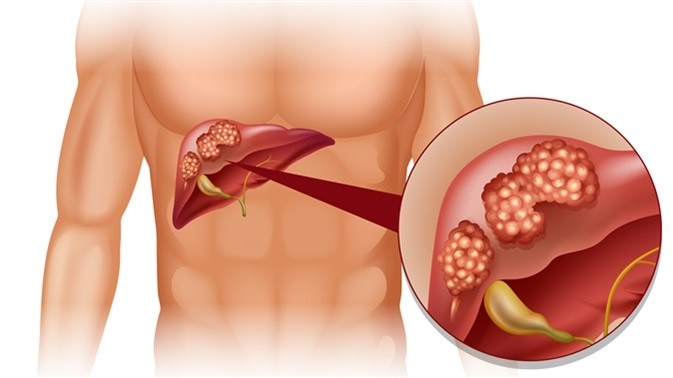
Liver cancer is a malignant tumor that develops in the tissues of the liver. This is considered as primary liver cancer. Liver cancer can also be as a result of migration of cancer cells originating from an infected organ; lungs, breasts or intestines. Liver cancer is also called hepatocellular carcinoma or malignant hepatoma.
Liver cancer is the fifth most common cancer worldwide. 560 000 new cases are diagnosed each year. Most cases of liver cancer is diagnosed in Southeast Asia, mainly in China, Hong Kong, Taiwan, Korea, and Japan; and sub-Saharan Africa, with a predominance in Mozambique and South Africa.
Types of Liver Cancer
Depending on the cells or tissues affected, liver cancer is classified into several groups:
Hepatocellular carcinoma – this type of cancer develops in a group of liver cells called hepatocytes. Hepatocellular carcinoma is a common type of primary liver cancer, which is caused as a result of complications of a disease already existing in the liver gland.
Cholangiocarcinoma – also called bile duct cancer, cholangiocarcinoma develops in the ducts of the liver that carry bile to the small intestines. It can cause biliary obstruction (bile duct obstruction), hence the emergence of cholestasis syndrome.
Angiosarcoma – also known as hemangiosarcoma, angiosarcoma is a rare form of cancer that starts in the blood vessels of the liver. It is often caused by prolonged exposure to toxic metals.
Hepatoblastoma – although hepatoblastoma is a rare form of primary liver cancer, it is the most common type of liver cancer in children. It is characterized by a palpable liver mass and abdominal pain. Hepatoblastoma represents approximately 1% of all paediatric tumors with an annual incidence of 1.5 cases per million children younger than 4 years.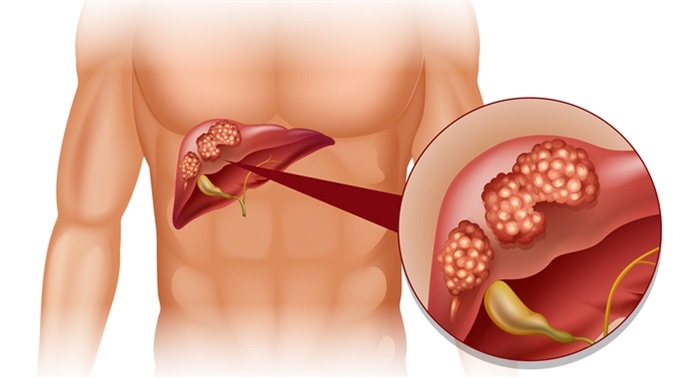
Liver Cancer Statistics
According to the National Cancer Institute (NCI), 22.620 people were diagnosed with liver cancer and intrahepatic bile duct in the US in 2009; about 18.160 died of the diseases. However, the incidence of liver cancer tends to vary with age and race. From 2002 to 2006, the median age at diagnosis for cancer of the liver and intrahepatic bile duct was 64 years of age.
Percentages and ages of people diagnosed were approximately:
- 1% under age 20;
- 0% between age 20 and 34;
- 7% between age 35 and 44;
- 3% between age 45 and 54;
- 6% between age 55 and 64;
- 5% between age 65 and 74;
- 8% between age 75 and 84
- 9% 85+ years of age.
Liver Cancer Causes
The liver is located in the abdomen under the right side of the diaphragm. It is the largest gland in your body. It plays important roles: secretion of bile for digestion, controlling and storage of many sugars and fats, storing vitamins and nutrients, filtering toxins in the blood, and synthesizing proteins essential for blood clotting. In addition, the liver participates in the transformation and assimilation of many drugs in your body.
Liver cancer occurs when there is a transformation of normal cells (hepatocytes) into malignant. The causes of liver cancer are not well known; however, most of the times, the disease is caused by excessive consumption of alcohol and chronic liver infections particularly hepatitis B and hepatitis C infection.
In developing countries in Asia and Africa, liver cancer is often the result of aflatoxin;a toxin that damages the liver and prevents it from neutralizing even small amounts of isopropyl alcohol. Aflatoxin is also a carcinogen; it can lead to liver cancer. It is produced by various species of microscopic fungi (mycotoxins) that like to thrive on seeds conserved in warm and humid areas.The two most common are Aspergillus flavus and Aspergillus parasiticus. Those mycotoxins are found primarily on bread, nuts, fruits, beer, wine vinegar, apple cider, and syrups.
Liver Cancer Risk Factors
Liver cancer is a multifactorial disease; its occurrence is not attributed to one factor. The most common factors that may increase your risk of becoming a victim of liver cancer include:
Being male – men are about three times more affected by liver cancer than women.
Age – in North America, Europe, and Australia, the diagnosis of liver cancer is frequently posed among people aged 63 years or more; in Southeast Asia and sub-Saharan Africa, however, the disease tends to affect people aged between 20 and 50 years old.
Liver disease – any chronic liver disease that is linked to excessive consumption of alcohol and hepatitis viruses B and C can lead to the development of liver cancer.
Obesity – being obese or overweight increases the chance of having many types of cancer, including liver cancer.
Diabetes – studies have shown a higher risk of liver cancer among diabetic people than those who are non-diabetics.
Hemochromatosis – this is a hematological disease characterized by excessive absorption of iron by the intestine causing its accumulation in certain tissues and organs.Having hemochromatosis put you at a higher risk of liver cancer. In addition, if you suffer from autoimmune hepatitis or Wilson’s disease, you have an increased risk of liver cancer.
Alcohol – if you consume daily for many years a large quantity of alcohol, you not only increase your risk of liver cirrhosis but also liver cancer.
Cirrhosis – liver cancer develops most often in liver affected by cirrhosis.
Nonalcoholic fatty liver disease (NAFLD) – any fatty inflammation of the liver, even when is not caused by excessive alcohol consumption, can foster the development of cancer cells in the liver gland.
Liver Cancer Symptoms
During its early development, liver cancer may cause no signs or symptoms. Even when there are symptoms, they are fairly discreet and can usually go unnoticed for a long period of time. In most cases, the cancer is discovered incidentally during an examination done for another medical condition or during regular check up to monitor cirrhosis.
When symptoms finally emerge, liver cancer tends to cause pain in the upper right of the abdomen and sometimes the presence of a palpable mass in the abdomen, just below the rib cage. As the disease worsens, the following symptoms can occur:
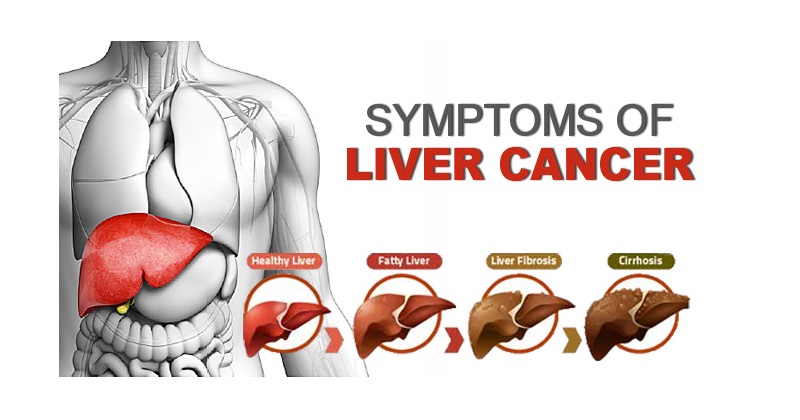 Fever
Fever- Nausea
- Weakness
- Difficulty breathing
- Loss of appetite
- Bloating
- Chronic fatigue
- Dark urine
- Gray stool
- Abnormal weight loss
- Yellowing of the skin and whites of the eyes.
Liver Cancer Complications
At a later stage when the tumor becomes diffuse or large, the cancer pain will intensify and cause serious complications:
- Confusion
- Internal bleeding
- Swelling of the spleen
- Fluid accumulation in the liver and intestines
- Increased abdominal girth.
Liver Cancer Diagnosis
Your doctor can begin the diagnosis by asking you questions about your experience with the symptoms. He will seek to know your medical history and your family’s. In addition, your physician will examine your body especially your abdomen, your skin, and eyes for signs indicating the presence of liver cancer. However, these procedures cannot confirm the diagnosis; other medical techniques such as blood tests, imaging techniques, and biopsy should be performed.
Blood tests – blood analysis can be recommended to measure levels of alpha-fetoprotein (AFP) in your blood. Alpha-fetoprotein is a plasma-protein normally produced by a fetus during its development.It is however a tumor marker in adults. AFP is often synthesized by certain liver tumors.The diagnosis is confirmed if the rate is higher than 400 ng/mL, in case of cirrhosis and nodule over 2 cm. In addition, the blood test can assess your liver function, and reveal liver function abnormalities.
Imaging Techniques – your doctor will recommend imaging tests such as x-ray, ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI) to visualize your liver. During the exams, your physician will inject an opaque dye into your arteries and veins of the liver to visualize its shape and size, and possibly discover abnormalities.
Liver metastases (cancer that has spread to the liver from another organ or tissue) are much more common than primary liver cancer. Therefore, your physician may also analyze your other organs to determine if you have a primary or secondary liver cancer.
Biopsy – even if the imaging techniques have revealed an abnormality in your liver, it is not sufficient to establish the diagnosis; a liver biopsy is necessary. A biopsy is important to confirm accurately the diagnosis of a primary liver cancer. This intervention is even more important if the results of blood tests and imaging techniques are inconclusive.The biopsy involves removing cells or tissues from your liver to examine under a microscope. However, a liver biopsy can lead to bleeding, bruising or/and infection.
Liver Cancer Stages
After the diagnosis is confirmed, your doctor will determine the stage of cancer. Staging the cancer is an important step.It helps your health care provider to choose the most effective treatment. In general, the stage of liver cancer is determined by the size of the tumor and its degree of spread within your body. To confirm with certainty the stage of a liver cancer, your physician may perform surgery, additional testing or removal of some lymph nodes near the tumor.
There are several methods used to define the stage of a liver cancer. The most common is the use of Roman numerals I, II, III and IV, which reads as stage I, stage II, stage III, stage IV. A higher number indicates a more serious liver cancer.
Carcinoma in situ (CIS) – also called stage 0, carcinoma in situ is the genesis of the cancer cells.
Stage I – at stage 1, the cancer is located in the liver without invading any blood vessels.
Stage II – at this stage, the tumor has grown to affect nearby blood vessels. The cancer can be multiple small tumors in your liver.
Stage III – the size of the tumor has increased; cancer has spread to nearby blood vessels, and/or nearby organs such as gallbladder.
Stage IV – at stage 4, cancer has formed several larger tumors in the liver and has spread from the liver to remote sites.
Liver Cancer Treatment

Once your doctor knows the type and stage of your cancer, he will determine the most appropriate treatment to fight the tumor. In addition, he will evaluate your health, age and other problems that may interfere with the treatment. In most cases, you will receive a combination of therapy. For primary liver cancer, treatment may include the following:
Partial hepatectomy
This surgical intervention is performed to remove a portion of the liver. Partial hepatectomy cannot be used in all liver malignancy.Generally, it is reserved for tumors less than 5 cm in diameter, or if cancer has not invaded the great vessels. Partial hepatectomy can also be performed if there is no metastasis outside the liver. 5 to 10% of cases of liver cancer are treated effectively with partial hepatectomy.
Liver transplant surgery
If the cancer is small, even if it is associated with cirrhosis, your surgeon may perform a liver transplant. It is a radical operation during which, your diseased liver is replaced with a healthy liver obtained from a donor. Liver transplantation can provide good results for some patients, but there are contraindications and waiting time is often long. In addition, you will have to take immunosuppressant drugs for the rest of your life after the transplant, which often cause serious health problems.
Radiofrequency ablation
If the transplant is not possible, your doctor can use electric current to heat and destroy the cancer cells; this therapeutic method is called radiofrequency ablation.
Chemoembolization
During the chemoembolization, your doctor blocks all blood supply to the tumor and injects powerful chemotherapy drugs directly into the arteries of the liver to facilitate the destruction of the cancer cells. Chemoembolization must be repeated every two to four months.
Radiation therapy (Radiotherapy)
Radiation therapy is a local regional treatment which consists of using high-powered energy beams to destroy cancer cells. Radiation therapy can shrink the tumor and reduce pain associated with cancer, but radiation therapy is effective in only a small percentage of patients. Most liver cancers are treated ineffectively with radiotherapy.
Injection of alcohol into the tumor
If you were diagnosed with a small-sized liver cancer, or in case there are few small tumors in your liver, repeated injections of alcohol directly into the tumor can lead to necrosis of cancer cells. This therapy rarely leads to complete recovery.It is a palliative treatment aimed at prolonging the life of liver cancer patients.
Cryoablation (freezing cancer cells)
Cryoablation is a new therapeutic method consisting of using extreme cold to destroy primary tumors and inoperable metastases. Cryoablation can be used as a unique therapy, or in combination with other therapies such as surgery, chemotherapy, or other standard treatments.
Liver Cancer Survival Rates
After the treatment, cancer can relapse. A second tumor often develops in the modified tissue remaining after the operation. Nearly half of patients who were operated for a smallsized tumor survive five years after the surgery.
Your chances of surviving depend largely on the stage of the tumor at diagnosis, your lifestyle, and age. The stage distribution based on Summary Stage 2000 shows that:
- 37% of liver and intrahepatic bile duct cancer cases are diagnosed while the cancer is still confined to the primary site (localized stage);
- 26% are diagnosed after cancer has spread to regional lymph nodes or directly beyond the primary site;
- 19% are diagnosed after cancer has already metastasized (distant stage)
- and for the remaining 18%, the staging information was unknown.
The corresponding 5-year relative survival rates were:
- 7% for localized;
- 5% for regional;
- 4% for distant;
- 8% for unstaged.
However, the survival rate tends to differ from one race to another. The overall 5-year relative survival rate for 1999 to 2005 was 13.1%. Five-year relative survival rates by race and sex were:
- 4% for white men;
- 6% for white women;
- 3% for black men;
- 0% for black women.
Liver Cancer Prevention
The best way to prevent the development of cancer in your body is to live a healthy lifestyle. Even if you are not at risk, you can have cancer if you continue to expose yourself to carcinogens.
Liver cancer is not attributable to one cause or factor; several factors can cause the formation of cancerous cells in your liver. Some risk factors such as sex and age are impossible to change.Others causative factors, however, can be prevented. If you want to prevent liver cancer and many other cancers, it is important to:
- Not consume alcohol regularly and/or in large quantity.Doing so helps you prevent not only liver cirrhosis but also liver cancer
- Not exposing yourself to aflatoxins and this precaution is even more important if you live in Asia or Africa
- Avoid tobacco smoke, including second-hand smoke
- Maintain a healthy weight
- Reduce your exposure to toxic chemicals
- Reduce your exposure to ultraviolet (UV) radiation
- Exercise regularly
- Practice safe sex
- Keep your immune system healthy
- See your doctor if the color of your eye and/or skin is yellowish
- Tell your doctor or dentist of any change that indicates the presence of cancer
Adopt a healthy diet: a diet containing 5 to 10 servings of fruits and vegetables a day may help prevent the occurrence of many cancers. Increase the following foods in your diet:
- Avocados
- Blueberries
- Black Raspberries
- Curcumin
- Flax
- Garlic
- Papaya
- Pomegranate juice
- Tomatoes
- Soy products
- Grapefruits, oranges and other citrus fruits
- Cruciferous vegetables (broccoli, cauliflower, kale, Brussels sprouts, and cabbage)