Table of Contents
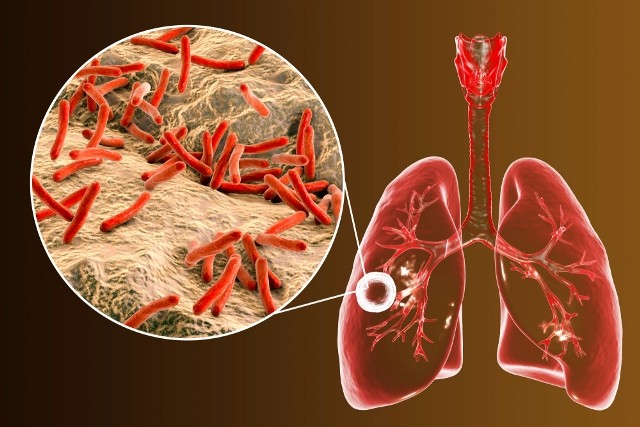
 Tuberculosis (TB) is a serious disease caused by the bacterium Mycobacterium tuberculosis, commonly called Koch’s bacillus. Tuberculosis is highly contagious – it spreads from one person to another through microscopic droplets released into the air. Despite advances in medical science, TB remains a life threatening disease killing thousands people every year.
Tuberculosis (TB) is a serious disease caused by the bacterium Mycobacterium tuberculosis, commonly called Koch’s bacillus. Tuberculosis is highly contagious – it spreads from one person to another through microscopic droplets released into the air. Despite advances in medical science, TB remains a life threatening disease killing thousands people every year.
The disease affects mostly the lungs (pulmonary tuberculosis); however, other organs may be also subject of tuberculosis: bone (Pott’s disease), the kidneys (renal tuberculosis), the intestines (intestinal tuberculosis) the genital organs (genital tuberculosis), the meninges (tuberculous meningitis, TB meningitis or tubercular meningitis) and the skin (cutaneous tuberculosis).
Although there are effective treatments against TB, some people develop a form of TB called multi-drug resistant tuberculosis.
Multi-drug resistant tuberculosis (MDR-TB) – MDR-TB is a form of tuberculosis that occurs when the treatment is noit followed properly; this may be due to negligence or lack of information. Most of the times, multi-drug resistant tuberculosis occurs when patients fail to take all the medications regularly and finish the treatment as prescribed by the health care provider. It may also be due to the fact that the doctor does not prescribe the appropriate medications. In poor countries, MDR-TB can occur because patients are prescribed ineffective drugs.
Multi-resistant TB is a dangerous form of tuberculosis. It is resistant to at least isoniazid and rifampicin, the two most effective TB drugs. When you have multi-drug resistant tuberculosis, the tuberculous bacteria multiply irreversible in your body. To prevent this form of tuberculosis, it is extremely important to follow your treatment until the end and as prescribed.
Epidemiology
Incidence of tuberculosis is increasing over the past fifteen years. According to the World Health Organization (WHO), every second a new person is infected with TB. 5 to 10% of people infected become tuberculous and are capable of transmitting the disease to another person. There are about 10 million new cases of TB each year worldwide; at least 3.9 million of them transmit the germs to other individuals; however, not all of them will develop the disease. According to WHO, the number of deaths due to TB each year is estimated at 2 million, about 80% of all these victims live in sub-Saharan Africa and Asia.
Tuberculosis Warning Signs and Symptoms
You can be affected with tuberculosis for a long period of time without showing any symptoms. In fact, at early stage, tuberculosis symptoms can be confused with those of respiratory system diseases. In general, pulmonary tuberculosis symptoms include:
- Persistent mild fever (38-38,5 ° C)
- Chills
- Cough
- Bloody sputum (spitting up blood)
- Loss of appetite and weight loss
- Night sweats
- Joint pain
- Pain in the chest during breathing or coughing
- Pain in the spine.
Tuberculous meningitis is a rare form of tuberculosis in which the Mycobacterium tuberculosis affects the meninges; it is characterized by:
- Persistent fever
- General health deterioration
- Weight loss
- Disturbances of consciousness
- Fatigue
- Persistent headache
- Diplopia – double vision, which gives perception of two images for one object
- Seizure
- Vomiting
- Photophobia – inability to bear the light.
Cutaneous tuberculosis – This is a very rare form of tuberculosis found especially among poor children, immuno-suppressed individuals (AIDS patients for instance) and very elderly. It is characterized by purplish or brownish-red warty growth which, most often, develops on the knees, elbows, hands, feet and buttocks. Cutaneous tuberculosis is often fatal despite advanced treatments. The Lesions can persist for years, leading to disfigurement and sometimes skin cancer.
Renal tuberculosis and Tuberculosis of the spine – other forms of tuberculosis may have symptoms slightly different. For instance, renal tuberculosis can cause kidney pain and hematuria (blood in your urine) and tuberculosis of the spine (Pott’s disease) can cause bone pain or back pain.
Tuberculosis Causes and Risk Factors
Tuberculosis is highly contagious. When an infected person coughs, sneezes, talks or spits, she/he releases in the air tiny droplets contaminated with the Koch’s bacillus. The TB bacteria remain suspended in air; you just need to inhale some to be infected. It is estimated that a person with active TB can affect on average 10 to 15 other people per year.
However, being infected by the germ does not necessarily mean that you will develop tuberculosis. Your immune system fights against the TB germ and prevent its development. This phase of the TB is called latent tuberculosis (latent TB). However, if your immune system is too weak to kill the bacterium, you develop the disease; this phase is called active tuberculosis (active TB).
Only those who have active TB are contagious. That is, if you have a latent or inactive form of TB, you do not represent any risk of contamination to others. Similarly, if you have active tuberculosis, and you follow your medication as you should, nobody can be contaminated by you. In other words, following your treatemt proplerly not only can save your life but also the life of every one who comes in contact with you.
Risk factors
Several factors can increase your risk of having tuberculosis:
- Malnutrition
- Immunosuppression (weakened immune system)
- Intravenous drug use
- Heavy alcohol consumption
- Being elderly
- Being homeless
- Traveling to places where TB is very frequent
- Direct contact with infected people
- Medical professions that put you in direct contact with TB patients
In addition, environment and certain diseases can increase your risk of contracting tuberculosis:
Environment – tuberculosis is more common in the region of Africa and Southeast Asia. In 2004, tuberculosis cases in these regions represent 33% of the global incidence, according to World Health Organization (WHO). The estimated incidence in sub-Saharan Africa is almost twice of that of Southeast Asia, with nearly 400 cases per 100 000 inhabitants.
Diseases – immunosuppressive diseases such as HIV/AIDS seems walk in pairs with tuberculosis. In addition, HIV/AIDS increases your chance of dying from the disease. For example, if you are infected with the TB germ, while positive for HIV, you have more risk of contracting TB than someone infected with TB but who is not a HIV positive.
Diagnosis
To determine if you have latent TB or active tuberculosis, your doctor may recommend some medical tests such as intradermal test (skin test), chest X-ray and sputum examination
Intradermal test (skin test) – The skin test is done to detect in your body the presence of bacteria specific to tuberculosis. The most common method is the Mantoux test, also known as the Mantoux screening test or Tuberculin Sensitivity Test.
During the test, a small amount of Tuberculin, Purified Protein Derivative (PPD) is injected under your skin, mostly below the skin of your inside forearm. If you have tuberculosis, the injection will cause a skin reaction within 2 days; you will develop a red bump where the needle entered the skin. However, the Koch’s bacillus should be in your body for several weeks for the skin test to be positive.
In addition, the Mantoux test is not always accurate; it may indicate a positive result even if you do not have TB. This can happen if
- You are infected with another type of mycobacterium
- You have been vaccinated with Bacillus Calmette–Guérin (or Bacille Calmette–Guérin, BCG)
- Your immune system is weak due to some medical conditions such as AIDS, cancer, or taking certain medications.
In addition, the skin test can not reveal if the TB is inactive or active. Therefore, the Mantoux test must be accompanied by other medical examinations such as polymerase chain reaction, chest x-ray and sputum analysis.
Polymerase Chain Reaction (PCR) – PCR is a rapid and sensitive method of molecular biology in vitro DNA amplification to detect the presence of the tuberculosis causative bacteria in your system. With this technique, the specialist can amplify a desired DNA sequence of any origin (virus, bacteria, etc.) hundreds of millions of times within hours. Besides TB, this technique can help your physician to detect HIV virus and hepatitis viruses B, C and D.
Chest x-ray – After a positive skin test, your doctor may recommend a chest x-ray to detect presence of:
- Fluid in your lungs
- White spots in your lungs
- Bacteria surrounded by macrophages
- Nodules or cavities caused by bacteria.
If the X-ray shows any of the above signs, your doctor may take a tissue sample to examine under a microscope (biopsy). In some cases, a CT scan or an MRI can be done to allow your doctor to examine your lungs with more accuracy.
Sputum analysis – a sputum analysis is another exam that your doctor may recommend if the x-ray reveals clinical signs of tuberculosis. A lab specialist will test a sample of the mucus from your lungs to look for TB bacteria. Sputum analysis is always accompanied by a chest X-ray to help your physician detect pulmonary TB.
Tuberculosis Treatment
Depending on the damage of the disease in your lungs and how your body reacts to the medications, TB treatment can include many phases:
Phase 1 – In general, your doctor will use the following four antibiotics to treat your TB: Rifampin, Isoniazid, Pyrazinamide, And Ethambutol. Throughout the treatment, your doctor will do a series of tests to monitor youe body and identify the bacteria resistance to the drugs. According to the results of these tests, ineffective drugs will be replaced by others. To be effective, drugs must be taken daily for a minimum period of six months. In addition, during the treatment, it is important to avoid alcohol and excessive sexual intercourse. It is also necessary to sleep at least 8 hours every night.
Phase 2 or multidrug-resistant TB (MDR TB) treatment – unfortunately, sometimes the bacteria are resistant to Isoniazid and Rifampin, and lead to a form of tuberculosis called multidrug-resistant TB (MDR TB). In this case, your doctor will use other drugs such as Ethionamide, Cycloserine and Kanamycin to fight the disease. However, these medications are less effectiveness; they must be taken over a longer period of time, sometimes up to two years. They are also more likely to cause side effects:
- Dark urine
- Persistent fever
- Loss of appetite
- Nausea or vomiting
- Skin discoloration (jaundice)
- Tenderness or soreness in your abdomen
- Blurred vision or colorblindness.
If you are infected by a strain resistant to all usual drugs, you’ll be recommended to take stronger antibiotics. The duration of treatment can last up to 2 years. In addition, these drugs are often taken intravenously, and they cause more severe side effects than the usual medications.
Whether you feel good or have side effects, you must continue the treatment until the end to destroy all the bacteria. Interrupting the treatment before term can make the bacteria become resistant to the drugs you are taking.
Tuberculosis Prevention
Vaccination – The Bacillus Calmette–Guérin (or Bacille Calmette–Guérin, BCG) vaccine does not protect you against tuberculosis at one hundred percent; its effectiveness varies from 0% to 80%. In fact, it is no longer used in developed countries.
Early detection – If you are at risk of tuberculosis, it is important to undergo a skin test. Earlier the disease is detected, the more chance you have to be healed. If latent tuberculosis is diagnosed, your doctor will recommend a preventive treatment, which often includes only one drug. Rarely, two medications can be prescribed to be taken daily for six to nine months.
You are at risk if you have been in contact with a patient in active phase, or your family has a history of tuberculosis. Other preventive measures against tuberculosis and other contagious diseases include:
- Boost or keep your immune system healthy
- Exercise regularly
- Eat a healthy diet
- Do not smoke
- Do not drink alcohol excessively.
If you are already tuberculous (active tuberculosis), finish your entire course of medication. In addition, it is important during the first few weeks of treatment to:
- Not go to work or school
- Not sleep in a room with other people
- Not speak with others face to face closely
- Not wet kiss your partner
- Cover your mouth when you cough, sneeze or laugh
- Do not spit on the ground; wind can transport the germs to others.
References :
1 – sante.gouv.fr ; La politique de lutte contre la tuberculose en France
2 – Global tuberculosis control: surveillance, planning, financing. WHO report 2008. Geneva, World Health Organization (WHO/HTM/TB/2008.393). http://www.who.int/tb/publications/global_report/en/index.html
3 – Who: Global tuberculosis control 2008
4 – WHO ; Infection et transmission de la tuberculose
5 – http://www.voyageslouk.com/sante/tuberculose.htm
6 – ornl.gov; Mapping and Sequencing the Human Genome