Table of Contents
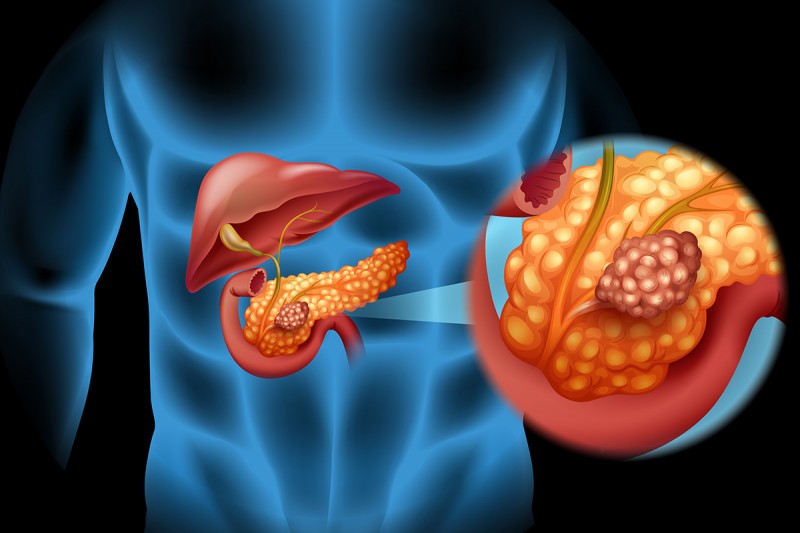
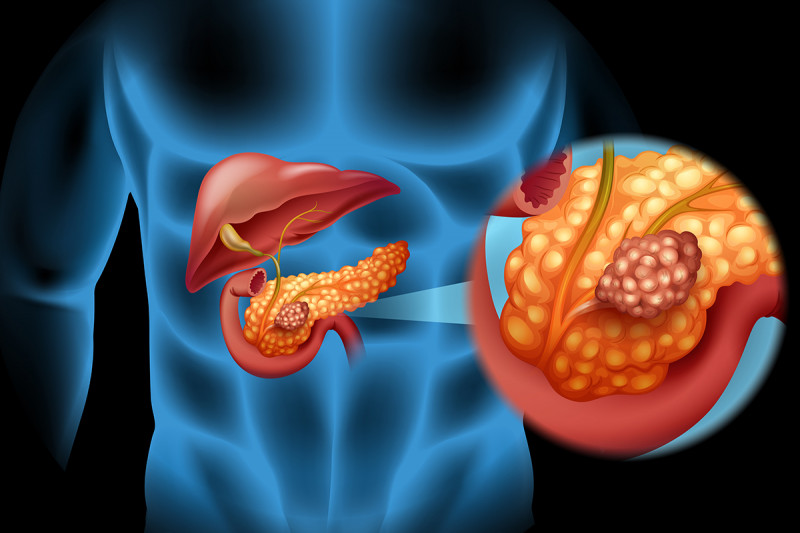
You have pancreatic cancer when there is a malignant growth in the tissue of your pancreas. Although the cancer can develop in different groups of cells in the pancreas, it often begins in the gland that secretes the digestive enzymes. Despite advances in medical science, your chances of recovering from pancreatic cancer are unfortunately low. The reason is that the moment you start experiencing symptoms, the cancer has often already formed metastases; it has spread into nearby lymph nodes, and sometimes the liver.
Your pancreas is a gland in your abdomen behind your stomach and above the kidneys. It is the second largest organ in your body after the liver. It plays two important functions:
- Exocrine function– this is the production of pancreatic enzymes (pancreatic juice) into the duodenum (the initial segment of the small intestine follows the stomach through the pylorus) by the duct of Wirsung (also called pancreatic duct); the juice involved in digestion of foods by breaking down the molecules more or less thick.
- Endocrine function– this function of the pancreas consists in the production of four hormones: insulin, glucagon, somatostatin and pancreatic polypeptide. After having discharged into the bloodstream, these hormones, primarily glucagon and insulin, provide concentration of blood glucose, and prevent the development of hypoglycemia (decreased level of blood glucose).
Pancreatic Cancer Statistics
Worldwide, over 216 000 new cases of pancreatic cancer are diagnosed each year; at least 188.000 people die of the disease. In 2007, pancreatic cancer was responsible for the fourth highest number of deaths among cancer deaths in North America. In the united Sates alone, it is estimated that 42,470 men and women (21,050 men and 21,420 women) were diagnosed with pancreatic cancer in 2009; about 35,240 died of it.
Incidence of cancer of the pancreas varies with age. From 2002-2006, the median age at diagnosis for cancer of the pancreas was 72 years of age; percentages and ages of people diagnosed were approximately:
- 0% under age 20;
- 4% between 20 and 34;
- 4% between 35 and 44;
- 6% between 45 and 54;
- 2% between 55 and 64;
- 1% between 65 and 74;
- 4% between 75 and 84;
- 8% 85+ years of age.
Pancreatic Cancer Causes
Pancreatic cancer occurs when there is an uncontrolled multiplication of cells in the pancreas. These cells all derived from a single clone; due to certain factors, these cancer-initiating cells, have acquired certain characteristics that allow them to divide indefinitely without going through natural death. Early cancer cells are confined to the tissue of the pancreas; as the tumor grows, some cancer cells can migrate from their original site to form metastases in other tissues in the body.
Usually, cancer cells grow within the pancreas. In most cases, the tumor develops in the ducts that carry the pancreatic enzymes to the duodenum; however, in a small group of individuals, sometimes the cancer cells begin in the portion of pancreas that produce insulin, islets of Langerhans.
There are several forms of pancreatic cancer, depending on the types of cells involved; the two main types are:
- Exocrine pancreatic cancer (adenocarcinomas)– adenocarcinomas account for nearly 95% of exocrine pancreatic cancer. Usually, this type of cancer is formed in the excretory duct of the pancreas which opens into the duodenum.
- Endocrine pancreatic cancer– also known as known as neuroendocrine tumor, or pancreatic islet cell tumor, endocrine pancreatic cancer refers to any cancer that develops in the hormone-producing cells of the pancreas. There are in total 5 subtypes of endocrine cancers of the pancreas, depending on the hormone-making cell affected:
- insulinomas– the cancer forms in the cells that produce insulin;
- glucagonomas– the cancer forms in the cells that produce glucagon;
- gastrinomas– the cancer forms in the cells that produce gastrin;
- somatostatinomas– the cancer forms in the cells that produce somatostatin;
- VIPomas– also known as Verner Morrison syndrome, VIPomas forms in the cells that produce vasoactive intestinal peptide (VIP).
Pancreatic Cancer Risk Factors
Although the following conditions are suspected, pancreatic cancer can occur in absence of all known risk factors:
- Obesity– being obese increases the risk of all cancers, including pancreatic cancer
- Age– pancreatic cancer is more common among people in their sixties
- Gender– pancreatic cancer affects slightly more men than women.
- Race– African-American are more victim of pancreatic cancer than whites are.
- Smoking– cigarette smoke (including second hand smoke) increases your risk of developing pancreatic cancer; In fact, pancreatic cancer is two to three times more common among smokers.
- Unhealthy diet– consuming diets low in vegetables and fruits and high in red meat and saturated fats puts you at increased risk of developing pancreatic cancer.
- Heavy consumption of alcohol– chronic and excessive consumption of alcohol is a serious risk factor for pancreatic cancer.
- Certain diseases– diabetes mellitus, gingivitis or periodontal disease are shown to be associated with some cases of pancreatic cancer.
- Chronic pancreatitis– the risk of pancreatic cancer in individuals with familial pancreatitis is particularly high.
- Infection– certain infection such as helicobacter pylori infection is suspected in the formation of cancerous cells in the pancreas.
- Family history– about 10% of pancreatic cancers have a hereditary connection. Some family history of genetic syndromes that have been associated with pancreatic cancer include:
- hereditary non-polyposis colon cancer, also called Lynch syndrome
- familial adenomatous polyposis (FAP), an inherited disorder characterized by presence of malignant tumor in the large intestine (colon) and rectum
- hereditary intestinal polyposis syndrome,a rare autosomal dominant genetic disease characterized by the development of benign hamartomatous polyps in the gastrointestinal tract and change in epidermis color of the lips and oral mucosa
- Autosomal recessive ataxia-telangiectasia and autosomal dominantly inherited mutations in the BRCA2 gene and PALB2 gene
Pancreatic Cancer Symptoms
The symptoms of pancreatic cancer usually occur after the disease is already advanced. In most cases, the time that you feel symptoms, the cancer has often already formed metastases; it has invaded nearby lymph nodes, and sometimes the liver. Common symptoms of pancreatic cancer include:
- weight loss
- loss of appetite
- nausea and Vomiting
- diarrhea /constipation
- depression
- Pain in the upper abdomen
- yellowing of the skin and the whites of the eyes (jaundice)
Pancreatic Cancer Complications
Pancreatic cancer is often associated with complications; the most common include:
- dark-colored urine and very pale stools
- severe abdominal pain, mostly when the tumor presses on the nerves in your abdomen
- Bowel obstruction –this occur when the cancer presses on the small intestine (duodenum), and blocks the flow of digested food from your stomach into your intestines.
Pancreatic Cancer Diagnosis
There is no systematic screening for pancreatic cancer. Your doctor will collect samples of blood; perform medical imaging techniques, including ultrasound, CT scan, MRI, endoscopy, endoscopic ultrasonography and percutaneous transhepatic cholangiography (PTHC or PTC). However, to confirm the diagnosis with certainty, a biopsy is also necessary.
Blood tests – Your doctor may recommend a sampling of your blood to detect anomalies and the presence of cancerous signs in the pancreas. Certain biomarkers levels such as antigen CA19.9 are increased in most cases of large tumors in the liver and pancreas. It is an important examination in the diagnosis of pancreatic cancer; however, CA19.9 is not sensitive for detecting small tumors. In addition it is not completely reliable; its elevation may be due to a benign but not malignant tumor. CA19-9 can be realized before, during or/and after the treatment.
Ultrasound – this medical imaging technique uses painless high-frequency sound waves to visualize various organs in your body including pancreas. It involves applying an ultrasound sensor (transducer) on your upper abdomen in order to obtain images of the pancreas. The transducer emits ultrasonic through the tissues of the pancreas and are returned as an echo. The result is then collected and analyzed by a computer system that transmits a live image on a video screen.
Ct scan – a scanner is the use of x-rays to create images of your internal organs. It can detect abnormalities not visible on standard x-ray and ultrasound. The CT scan allows not only to confirm the presence of the tumor but also to highlight lymph nodes or liver metastases.
Magnetic Resonance Imaging (MRI) – an MRI with injection of contrast allows your physician to visualize organs of the inside of your body. In the case of a pancreatic cancer diagnosis, it can analyze the structure of your pancreas, to search for abnormalities, inflammation, and highlight the presence of the tumor. In addition, the MRI can help your doctor to know the exact size and extent of the tumor.
Endoscopic retrograde cholangiopancreatography (ERCP) – with this imaging technique, your doctor can see inside your stomach and duodenum, and possibly detect diseases; it combines the use of endoscopy and fluoroscopy. ERCP is used to diagnose and treat certain problems of the liver, gallbladder, bile ducts, and pancreas: gallstones, inflammatory tissues and cancer. During the procedure, your doctor injects dyes into the ducts in the biliary tract and pancreas so they can be visible on x-rays.
Endoscopic ultrasound – an endoscopic ultrasound is an exploration of the digestive system that combines endoscopy and ultrasound; this exam is very important in cases of small-size pancreatic tumor. During the procedure, a miniaturized ultrasound probe – attached to the end of a flexible endoscope – is positioned near the body to examine which allows your doctor to search or explore lesions in the gastrointestinal tract or adjacent organs including the pancreas. Endoscopic ultrasound also allows, when it is appropriate, puncture to the tumor to obtain sample for lab analysis (biopsy).
Percutaneous transhepatic cholangiography (PTHC or PTC) – PTC is a radiological technique often performed to examine the anatomy of the biliary tract. During the exam, your doctor injects a contrast agent (dye) into the bile in the liver. Afterwards, a special X-ray machine called fluoroscopy is used to track the travel of the dye. With a PTC, your physician can determine whether there is a blockage in the liver or the bile ducts.
Biopsy – even if the other diagnostic techniques have revealed the cancer, a biopsy is usually required to confirm the diagnosis with certainty. A biopsy of the pancreas is to remove cells or pancreatic tissue to examine under a microscope. There are many types of biopsies; the type used depends on where the tumor is located. However, whatever the method used, it must be done carefully so it does not promote the spread of cancer cells.
Pancreatic Cancer stages
Once the cancer is detected, your doctor will determine its stage. Most of the times, he will use the result of the biopsy associated with those of the imaging techniques to determine the stage of the cancer. In general, Pancreatic cancer develops in four stages:
- Stage I –at this early stage, the tumor is confined to the pancreas;
- Stage II –the cancer has reached nearby tissues or organs of the pancreas; the cancer may have spread into the lymph nodes;
- Stage III –at stages 3, the cancer has affected blood vessels around the pancreas, and may have spread to the lymph nodes;
- Stage IV –at this final stage, the cancer has spread into distant sites beyond the pancreas: liver, lungs, peritoneum, etc. Your chance to survive has decreased considerably.
- Recurrent– the cancer has returned after treatment. In general, recurrent pancreatic cancer is more difficult to be treated.
Pancreatic Cancer Treatment

To determine the most appropriate treatment for your situation, your doctor will consider the stage and type of cancer you have. In addition, he will consider your age and your health in general. Knowing this information, he will be able to determine which treatment is most effective to fight the cancer. After all, you will be invited to participate in the final choice.
Pancreatic cancer treatment is primarily surgery; in most cases, particularly when the cancer is diagnosed at an advanced stage, chemotherapy as well as radiation therapy can be combined with surgery to increase your chances of surviving.
Surgical Treatment
Surgical removal is the most effective treatment for a cancer that is confined to the pancreas. Unfortunately, nearly 90% of pancreatic cancers are diagnosed at an advanced stage, making surgical intervention difficult or even impossible. Sometimes, the surgery is performed as a palliative treatment to improve the life of the patient. This is applicable in the case of a tumor compressing the duodenum, which makes difficult the passage of foods in the intestine. The surgery aims to derive the biliary duct or stomach directly into the small intestine.
Usually, one of these three types of surgery is performed to remove the cancer from the pancreas:
- Whipple’s surgery– this surgical procedure is performed in cases of a cancer located in the head of thepancreas, the widest part of the pancreas. In this case, your surgeon removes the head of the pancreas and part of the small intestine, bile duct and stomach. After the removal, your surgeon will connect the stomach to the intestine, as well as anastomosis of the bile duct into the small intestine; the remaining pancreas is connected to either the stomach or the small intestine, to allow the flow of bile and pancreatic juice into the gastrointestinal tract.
- Distal pancreatectomy– during the surgery, the body and tail of the pancreas are removed if the tumor is located in one of these two regions. In addition, your surgeon will remove your spleen.
- Total pancreatectomy– this is a major surgical intervention reserved for very advanced pancreatic cancer. During the operation, the entire pancreas, part of the small intestine, part of the stomach, bile duct, gall bladder, spleen, and nearby lymph nodes are removed. Total pancreatectomy is rarely performed, because it often leads to lifelong adverse effects – for instance, inability to produce pancreatic enzyme and insulin.
Radiotherapy (Radiation therapy)
Radiotherapy is use of ionizing radiation (subatomic particles or electromagnetic waves) to treat cancer. The therapy shrinks or eliminates the tumor by stopping the development or division of cancer cells. Unlike chemotherapy, which acts on cancer cells throughout the body, radiotherapy is a local treatment that acts on a specific area. The radiation is often performed after the surgery. Radiation therapy is painless procedure, and cause minimal or no side effects.
Pancreatic Cancer Chemotherapy
In the treatment of pancreatic cancer, chemotherapy is often used after the surgery. Chemotherapy can also be used to treat advanced pancreatic cancers for which surgery is not possible. Unlike surgery and radiotherapy, chemotherapy is a systemic treatment that affects the entire organism. The chemotherapy drugs designed to destroy cancer cells or prevent them from multiplying. These drugs can be taken by mouth, infusion or injection.
However, chemotherapy drugs affect both cancer cells and healthy cells that divide rapidly, which often lead to side effects:
- fatigue
- nausea
- vomitting
- hair loss
- abdominal pain
- and more…
Targeted Therapy
Targeted cancer therapy is less harmful to normal cells, and can be very effective in the treatment of pancreatic cancer. Targeted therapy drugs stop multiplication of cancer cells by interfering with specific targeted molecules that they need to survive. The drug used in the treatment of pancreatic cancer can be an antibody against a gene expressed at the surface or in the cancer cell, or a molecule capable of blocking the transmission of the signal of cell division. The drug may also be antibody directed against the new vessels produced by the tumor to feed. Targeted therapy can be administered sometimes alone, sometimes in combination with chemotherapy or radiation.
Pancreatic Cancer Prognosis
Pancreatic cancer prognosis depends on the extent of the tumor, its type and quality of surgery performed. The chances of surviving pancreatic cancer are often low because usually when symptoms appear, the tumor is already advanced and formed metastases in nearby lymph nodes or in the liver or other organs. In fact, only 5 to 10 percent of patients operated for pancreatic cancer are still alive five years after the surgery; some do not survive the surgery.
According to the National Cancer Institute, about 7% of pancreas cancer cases are diagnosed while the cancer is still confined to the primary site (localized stage); 26% are diagnosed after the cancer has spread to regional lymph nodes or directly beyond the primary site; 53% are diagnosed after the cancer has already metastasized (distant stage) and for the remaining 14% the staging information is unknown.
The corresponding 5-year relative survival rates were:
- 2% for localized;
- 7% for regional;
- 8% for distant;
- 9% for unstaged.
In addition, the survival rates vary with race and sex. The overall 5-year relative survival rate for 1999-2005 from 17 SEER (Surveillance Epidemiology and Ends Results) geographic areas was 5.5%. Five-year relative survival rates by race and sex were:
often lead to side effects:
- 5% for white men;
- 5% for white women;
- 5% for black men;
- 2% for black women.
Pancreatic Cancer Prevention
The only possible prevention for pancreatic cancer is to avoid known risk factors that can lead to its development, in particular:
- obesity
- smoking
- alcohol abuse
- Prolonged consumption of a diet rich in animal fats and low in fruit and vegetables.
Your lifestyle as well as your environment and your workplace may be open doors to development of several types of cancer, including pancreatic cancer. If you want to prevent the development of almost any cancer in your body, it is important to:
- adopt a healthy diet– a diet containing 5 to 10 servings of fruits and cruciferous vegetables a day can help prevent many cancers including pancreatic cancer.
- reduce your exposure to ultraviolet (UV) radiation from the sun or artificial tanning devices, such as tanning beds;
- tell your doctor or dentist of any change that indicates the presence of cancer;
- do not smoke and avoid second hand cigarette smoke;
- exercise regularly
- maintain a healthy weight
- limit your intake of alcohol
- Practice safe sex.