Table of Contents
Arteriosclerosis is a degenerative disease of the arteries. This degeneration occurs when there is destruction of muscle fibers that form the inner layer of the arteries, causing them to lose their elasticity and become narrowed.
Different Types of Arteriosclerosis
The term arteriosclerosis is often referred to two different diseases that can be easily misused: Arteriosclerosis (note the rio) and atherosclerosis (note the ro).
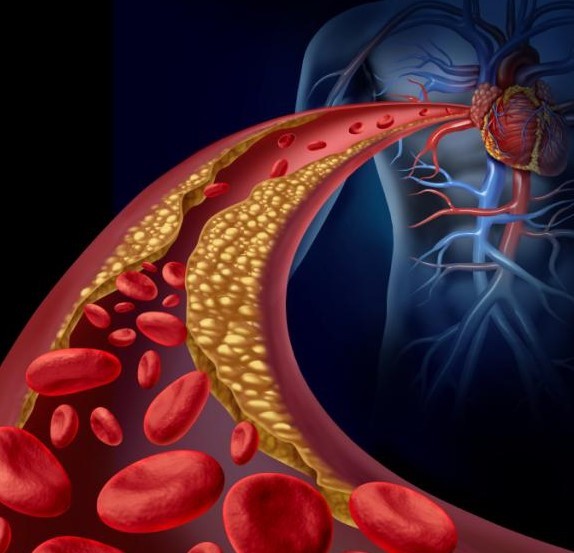
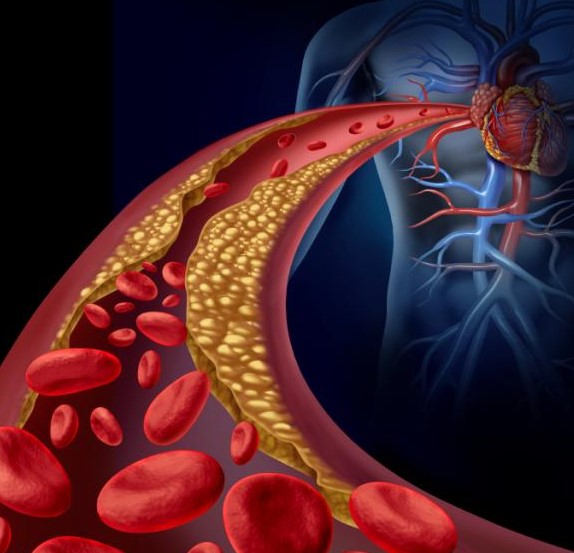
Arteriosclerosis – arteriosclerosis is an anatomical disorder of your arteries caused by accumulation of deposits of fat (especially cholesterol) in their wall. Those deposits lead to a narrowing of the arteries, impairing blood flow from your heart to other organs of your body
Although the buildup can be formed in any artery, the following are always the most affected: the coronary arteries (those of the heart), renal arteries, the arteries of the eye, the arteries of the lower limbs and the arteries of the brain.
Atherosclerosis – often associated with arteriosclerosis, this medical condition is characterized by the hardening of the inner layer of your arteries preventing blood circulation from left ventricle of the heart to the rest of your body. Atherosclerosis is the main factor of heart attack, stroke and arthritis of the lower limbs.
Atherosclerosis has been described accurately for the first time during the second half of the nineteenth century; however, that is in 1904 that the German Felix Marchand coined the term ‘atherosclerosis’ to refer to the disease.
Arteriosclerosis Causes and Risk Factors
The causes of arteriosclerosis are not well known. Nevertheless, researchers think a number of cardiovascular risk factors can contribute in developing the disease. As cardiovascular disease, arteriosclerosis can be caused by:
- Cigarette smoke
- Hypertension
- Unhealthy diet
- Diabetes
- Obesity
- High cholesterol in the blood
- Physical inactivity
- Family history of atherosclerosis

- Sex; men are more affected than women are
The disease progress is usually slow but gradual. It may start from childhood, and continue until adulthood without apparent symptoms.
Stress is also suspected in the development of arteriosclerosis. Stress tends to release adrenaline (a natural hormone your body produces when you are stressed or are physically exhilarating), which can cause spasms in the arteries. When stress is repeated too often, it can lead to high blood pressure (due to adrenaline hyper secretion) and arterial spasms; those two, in return, promote atherosclerosis.
Arteriosclerosis Warning Signs and Symptoms
Since arteriosclerosis is a gradual disease, it can be asymptomatic for years. You feel the symptoms only when the narrowing of the artery blocks the bloodstream either completely or quasi-totally. The symptoms are substantially the same as those of atherosclerosis:
Shortness of breath (dyspnea)
- Angina attacks
- Dizziness
- Chest pain
- Arrhythmia (irregular heartbeat).
Complications
If left untreated, the lesions may develop into myocardial infarction (heart attack), stroke, kidney failure, or arteritis (inflammation of the walls of arteries) of the lower limbs.
What is the diagnosis of Arteriosclerosis?
Arteriosclerosis can be detected clinically by palpitation of the arteries and blood test. Several blood tests can be done to detect increased levels of cholesterol and other clinical signs of arteriosclerosis. For more accuracy, your physician can recommend certain exams to estimate the location and spread of the disease. Some of the most common used are:
Coronary Angiography, to analyze the location and severity of the narrowing;
Vascular Ultrasound, a non-invasive procedure used to detect how blood flows through your arteries and veins;
Angioplasty, study of the blood vessels in your body; this medical procedure also allows your surgeon to remove buildup in the artery wall and restore blood flow.
Electrocardiogram (ECG) – this painless test records electrical activity of your heart, permitting your doctor to measure the electrical activity of your heartbeat.
Arteriosclerosis Treatment and Prevention
The treatment is primarily preventive and focuses on:
- Living a healthy lifestyle
- Mental relaxation
- Moderate physical activity
- Quitting smoking
- Avoiding stress
- Eating a healthy diet
Drugs therapy – to remove the plaques, drugs are sometimes necessary. Your doctor may prescribe you Anti-platelet medications (Cyclooxygenase inhibitors, Aspirin, etc.), Anticoagulants (warfarin, Heparin, etc).
Surgery – Depending on the result of the test and the efficacy of the medication, surgery may be required. Your doctor may suggest one of the following:
Angioplasty, dilation of narrowed or totally obstructed blood arteries;
Endarterectomy – a surgical procedure in which your surgeon removes fatty deposits in your blocked artery lining to restore blood flow;
Thrombolytic therapy – the use of drugs to break up or dissolve blood clots within a blocked artery;
Bypass surgery – this is a surgical procedure performed to allow blood flow around clogged arteries. This technique is done to replace a vessel or a portion of an obstructed vessel. Your surgeon interposes a tube or a synthetic fragment of vein to restore normal blood circulation. Bypass surgery is used when an artery is completely narrowed due to buildup of fatty deposits within the arterial wall