Table of Contents
Aortic Insufficiency
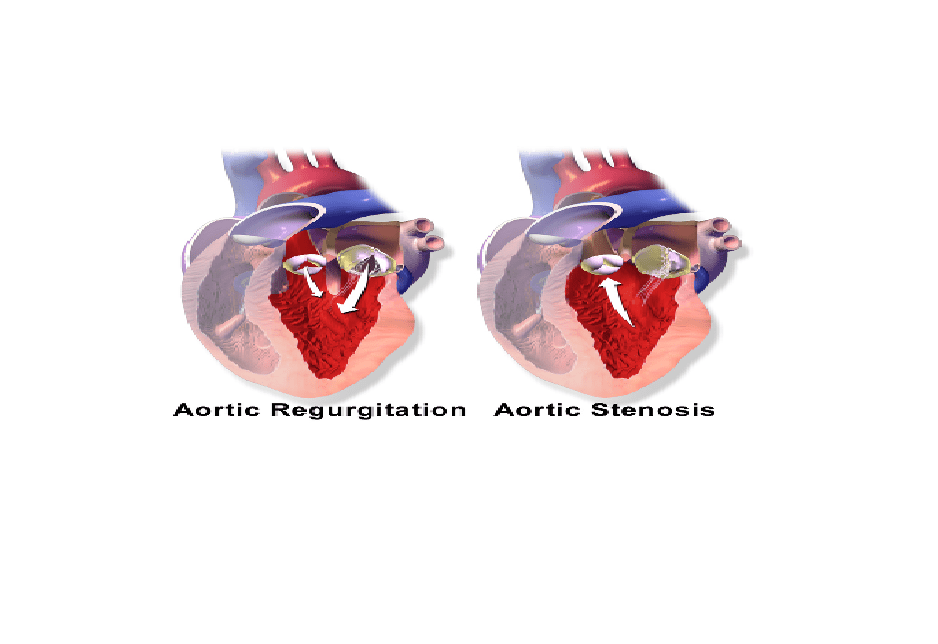
Aortic insufficiency, also known as aortic valve regurgitation or just aortic regurgitation, refers to an incomplete closure of the heart aortic valve, organ located between the left ventricle and aorta. This disturbance causes a reflux of blood from the aorta to the left ventricle during diastole.
 Regurgitation of blood from the aorta to the left ventricle will cause an overload of blood in the ventricle. This strain makes the heart muscle increase volume and expands gradually. Because the heart overworks to offset the outflow of blood in the ventricle, without an effective treatment, this disorder can lead to dilation and failure of the left ventricle. However, you can spend years with an aortic valve regurgitation without experiencing any symptoms. Over time, however, the ability of the left ventricle to expel blood is exhausted and the force of contraction decreases. Then, you start experiencing signs and symptoms of valve regurgitation.
Regurgitation of blood from the aorta to the left ventricle will cause an overload of blood in the ventricle. This strain makes the heart muscle increase volume and expands gradually. Because the heart overworks to offset the outflow of blood in the ventricle, without an effective treatment, this disorder can lead to dilation and failure of the left ventricle. However, you can spend years with an aortic valve regurgitation without experiencing any symptoms. Over time, however, the ability of the left ventricle to expel blood is exhausted and the force of contraction decreases. Then, you start experiencing signs and symptoms of valve regurgitation.
Aortic Regurgitation Causes
The aortic valve, consisting of three leaflets called cusps or sigmoid valves, serves to seal the heart valves when closed. The aortic valve is located between the left ventricle of the heart and aorta, and ensures the continuous flow of blood from the left ventricle into the aorta. To ensure this vital function, the heart produces two movements: systole and diastole.
During systole, the ventricle contracts, the intra-ventricular pressure exceeds the pressure in the aorta to open the aortic valve, allowing blood to exit. During diastole, however, the heart relaxes and the pressure decreases, the valve closes to prevent blood flow from routing to the ventricle.
However, certain anomalies of the aortic valve may odd the functions of the heart and make the valve incontinent. This gives rise to a backflow of blood from the aorta to the ventricle during closing and opening; this is called aortic valve regurgitation. Multiple causes may lead to aortic regurgitation;
Most common causes: congenital heart defect, aortic valve degeneration, Osler’s nodes associated with infective endocarditis, atherosclerosis, syphilis, aortic dissection, chest trauma (also known as thoracic trauma), ankylosing spondylitis (painful redness and inflammation of the eye), chronic hypertension, rheumatic fever, and certain autoimmune diseases such as:
- lupus erythematosus
- Takayasu’s disease
- rheumatoid arthritis.
Rare causes include:
use of Fenfluramine
reactive arthritis (Reiter’s syndrome)
psoriatic arthritis
ulcerative colitis
syphilitic aortitis
Aortic dissection
giant cell arteritis
myxoid degeneration in patients with Marfan syndrome
Ehlers–Danlos Syndrome (EDS or “Cutis hyperelastica”)
Osteogenesis imperfecta (Brittle Bone Disease or Lobstein syndrome)
Aortic regurgitation Symptoms and Warning Signs
Most of the times, in the genesis of the aortic regurgitation, it causes no symptoms; the disease is discovered during a diagnosis for breathlessness or/and chest pain, or during medical exams performed for other health problems.
During a physical examination with a stethoscope, your doctor can detect signs of arterial hyper-pulsatility such as full pulse, bounding pulse, and heart murmur. The cardiologist may notice an elevated systolic pressure and a decreased diastolic pressure. However, very often, these symptoms appear at an advanced stage of the disease.
As the disease progresses, you may feel at least one of the following symptoms:
- Headache
- Fatigue
- Weakness
- Fainting (rarely)
- Heart palpitations
- Rapid or irregular pulse
- Swollen ankles and feet
- Shortness of breath on exertion
- angina pectoris on exertion or at rest
- Sensation of a rapid, fluttering heartbeat.

Complications
Aortic regurgitation can be treated or cured permanently; an untreated or chronic aortic insufficiency, however, can cause serious complications:
- Difficulty breathing
- Endocarditis
- Pulmonary edema
- Left-sided heart failure.
Diagnosis
Your doctor can start the diagnosis by a physical examination, looking for evidence of a heart murmur, shortness of breath and others signs of aortic valve regurgitation. This procedure, however, is not enough to confirm that you have aortic regurgitation. Along with the physical exam, your doctor will recommend the following exams to confirm the diagnosis:
Exercise test – also called stress test, exercise test is a diagnostic technique allowing your physician to register your heart’s performance during the course of a calibrated exercise. It is used in the diagnosis of aortic regurgitation to determine if blood flow in your heart muscle is normal.
Chest X-ray – this method is performed to produce images of the heart muscle, lungs and bones forming the thoracic cage. It allows your doctor to detect abnormal shape of the heart, and discover if it is larger than normal. In addition, the chest x-ray helps confirm the presence of a valve disorder and provides important details about your heart condition and its severity.
Echocardiogram – During an echocardiogram, the technician uses ultrasound to create picture of your heart muscle. The waves recorded help your physician to determine the shape, texture and movement of the valves and the volume and function of the cardiac chambers. In addition, this imaging technique is performed to determine the risk of clots formation inside the heart.
Generally, an echocardiogram is recommended if during the physical exam, your cardiologist suspects that your heart produces abnormal sounds, or you experience palpitations, breathless or chest pain.
Electrocardiogram (ECG) – This test is done to study the functioning of your heart by measuring its electrical activity. Each heartbeat produces an electrical impulse in your heart that contracts the heart muscle so it pumps blood to the body. By measuring the time the electrical impulse takes to travel through the heart, your cardiologist can determine if the electrical activity is normal, fast or irregular.
In addition, electrocardiogram allows your cardiologist to determine if your heart is dilated or overworking. Your cardiologist will recommend an ECG if physical examination shows signs of arrhythmia, palpitations, dizziness, fatigue or chest pain.
Transesophageal echocardiography (TEE) – TEE can be performed to detect blood clots. As an echocardiogram, the TEE uses sound waves at high frequency (ultrasound) to examine the heart structures. During the procedure, your health care provider will administer a mild sedative to help you relax during the entire procedure. In some cases, you can be supplied with oxygen during the intervention. In general, transesophageal echocardiography lasts 40 minutes or less.
Cardiac catheterization – your doctor may recommend a cardiac catheterization if you have signs of heart valves malfunctioning or heart failure. It consists of introducing a thin catheter through your blood vessel in your arm or groin into your heart chambers to measure pressure and blood oxygen saturation level. In addition, this examination allows your doctor to detect reflux of blood from the aorta to the left ventricle.
Aortic insufficiency Treatment
The treatment depends largely on the severity of the disease. If you have an aortic valve regurgitation that causes mild or no symptoms at all, your doctor may prescribe you vasodilators, drugs capable of enlarging the size of vessels. Along with the medications, you will be recommended to see your doctor regularly so that he can observe the evolution of the disease. In case of complications or severe symptoms, surgery may be considered. However, whatever the type of treatment used, its goal is to restore the normal function of the aortic valve and thus eliminate the pathological reflux of the aorta to the heart. Along with the treatment, it is important to:
- Limit your efforts
- Eat a heart-healthy diet
- Decrease your salt intake
- Avoid cigarette smoking, including secondhand smoke
- Exercise regularly – fast walking is excellent
- Have a healthy weight.
Sometimes, drug therapy doesn’t work; surgery is the best option to stop the regurgitation. Your surgeon will consider a surgical therapy if symptoms are severe or if the disease is caused by a defect in the aorta.
Surgical Treatment
Aortic valve repair – this surgical procedure is performed to treat certain abnormalities of the aortic valve in order to stop backward blood flow. Instead of an aortic valve replacement, your surgeon may decide to make an aortic valve repair if the aortic valve is not completely damaged. However, this procedure is less frequent.
Valve replacement – this surgery is intended to replace the leaky aortic valve by an artificial valve, which can be tissue or mechanical. The tissue valve can be your own pulmonary valve (autograft) or from a donor such as a dead patient (Homograft) or an animal, pig or cow. The mechanical valve is usually a metal, it can last several years. However, you will need to take anticoagulant medications for life, because it is accompanied with an increased risk of blood clots forming in blood vessels.
Valve replacement is mainly reserved for elderly patients with a normal heart rhythm, or those who are unable to properly follow an anticoagulation treatment.
Aortic insufficiency Prevention
 The two best ways to prevent aortic valve regurgitation is by keeping your blood pressure under control and preventing rheumatic fever. Having healthy blood pressure levels requires regular exercise, consumption of healthy diet, avoidance of bad stress and cigarette smoke, including second hand smoke.
The two best ways to prevent aortic valve regurgitation is by keeping your blood pressure under control and preventing rheumatic fever. Having healthy blood pressure levels requires regular exercise, consumption of healthy diet, avoidance of bad stress and cigarette smoke, including second hand smoke.
If you have strep throat, see your health care provider and follow the treatment as prescribed. Rheumatic fever is often the consequence of untreated or poorly treated strep throat. Prevention of recurrences is based on oral or intramuscular injection of antibiotics for at least 5 months. Talk to your physician for more information on Aortic insufficiency prevention.
References :
1 – Tahar CHERIGUI, Université Paris12-Cnrs(Paris6): Etude Hémodynamique de la Valve Aortique Par Modélisation Numérique 3D
2 – Aortic regurgitation at Mount Sinai Hospital
3 – Connolly HM, Crary JL, McGoon MD, et al. (1997). “Valvular heart disease associated with fenfluramine-phentermine”. N. Engl. J. Med. 337 (9): 581–8. doi:10.1056/NEJM199708283370901. PMID 9271479.
4 – Weissman NJ (2001). “Appetite suppressants and valvular heart disease”. Am. J. Med. Sci. 321 (4): 285–91. doi:10.1097/00000441-200104000-00008. PMID 11307869
5 – Wilson W, Taubert KA, Gewitz M; et al. (October 2007). “Prevention of Infective Endocarditis: Guidelines from the American Heart Association” 116 (15): 1736–54. doi:10.1161/CIRCULATIONAHA.106.183095. PMID 17446442