Table of Contents
Heart Failure
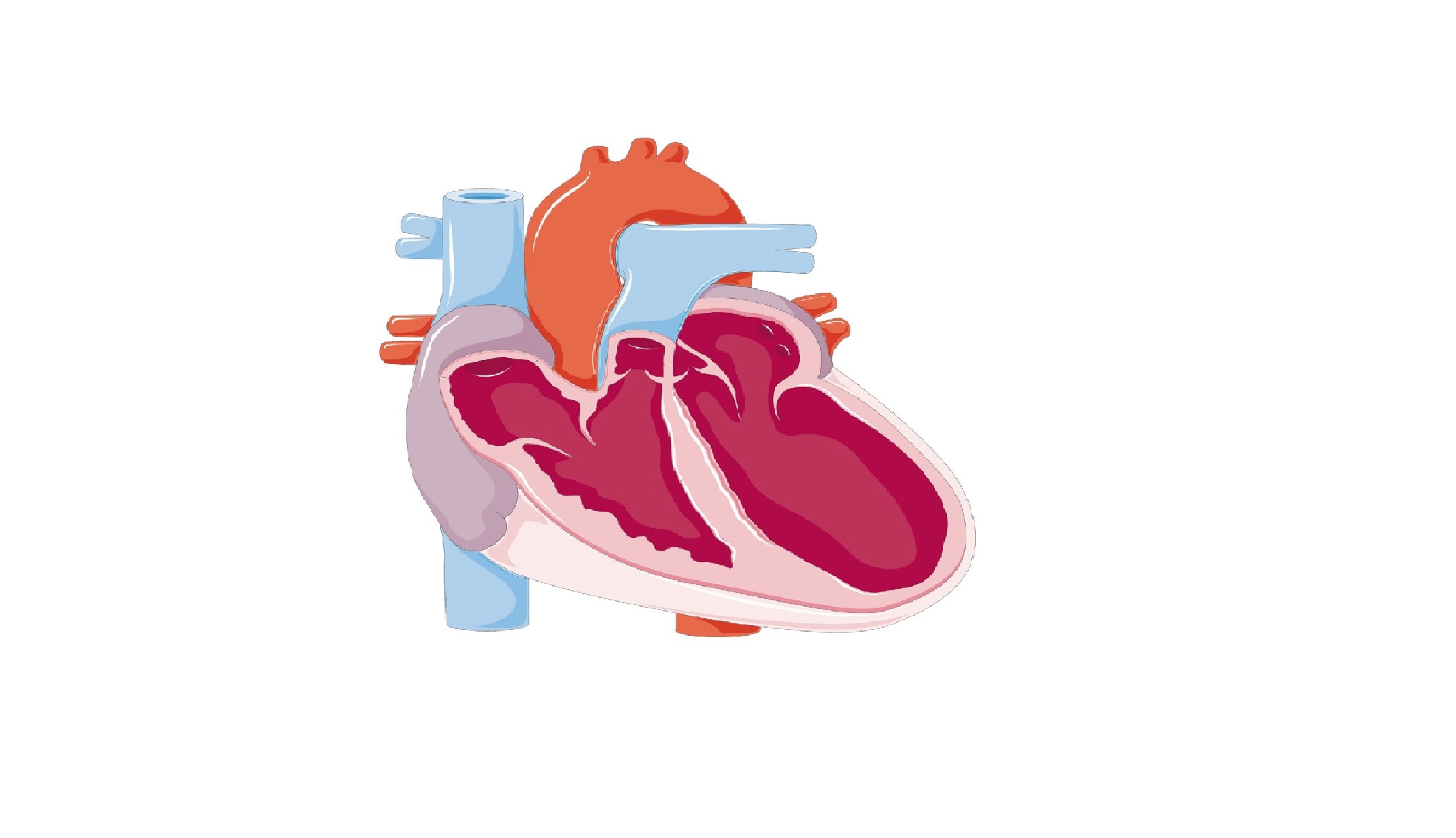
Heart failure, also known as Congestive heart failure, occurs when the heart is unable to propel blood out to the body to ensure the needs of the cells in oxygen and nutrients, without which they cannot live. This failure may be due to abnormal contraction of the ventricular heart muscle (systolic dysfunction) or abnormal filling during diastole (diastolic dysfunction); sometimes, both mechanisms occur.
A failure can affect different parts of the heart muscle:
Left-sided heart failure – this condition occurs when the left side of the heart cannot pump enough blood to other organs of the body. Left-sided heart failure is the most common form of congestive heart failure.
Right-sided heart failure – this is a condition in which the right side of the heart fails to efficiently pump blood that the body needs to function properly.
Systolic heart failure – systolic heart failure occurs when the heart’s lower chambers (ventricles) lose their ability to contract and pump out sufficient blood.
Diastolic heart failure – After each contraction, the ventricles then relax to re-fill with blood to prepare for the next contraction (diastole). Diastolic heart failure occurs when ventricles cannot completely relax and fill during diastole.
Incidence
Heart failure is a serious condition in the US and other developed countries. According to National Heart, Lung, and Blood Institute, nearly 5 million people in the United States have heart failure, leading to 300,000 deaths each year. The risk of congestive heart failure increases with age; heart failure affects about 1% of the population aged 50 and 10% of people aged 80 and over.
Congestive heart failure is a common disease all over the world. In addition to industrialized countries, developing countries feel also the effects of the disease. It is estimated that 17 million people worldwide suffering from chronic heart failure. Anywhere in the world, you can be a victim of congestive heart failure. The best way to prevent heart failure is to avoid or control all risk factors that can lead to it: coronary artery disease
- unhealthy diet
- high blood pressure levels
- physical inactivity
- cigarette smoke, including second hand smoke
- high cholesterol levels
- diabetes
- Obesity, etc.
Heart Failure Causes
The causes of heart failure vary slightly depending on the type of failure. Congestive heart failure can be acute or chronic:
Chronic heart failure – this is a long-term inability of the heart muscle to perform its function of pumping blood. Chronic heart failure is often associated with signs and symptoms that require immediate medical attention. If left untreated, the failure will lead to progressive destruction of the heart muscle; eventually, the heart will completely lose its ability to contact. The most common causes and risk factors of chronic heart failure include:
[row][double_paragraph]- Angina
- Rheumatoid arthritis
- Chronic anemia
- Previous heart attack
- Lupus complications
- Diabetes complications
- Coronary artery disease
- Untreated or poorly high blood pressure
- Injury or damage to the heart muscle
- Congenital heart defects
- Heart valve diseases
- Untreated or chronic sleep apnea
- Chronic kidney problems
- Alcohol abuse
- Persistent degenerative vascular disease
- Persistent abnormal heart rhythms
- Thyroid problems (hyperthyroidism, hypothyroidism)
- Swollen or inflammation of the heart muscle (myocarditis)
- complications of certain lung diseases such as pneumoconiosis and silicosis
- Complications of chronic lung disease leading to chronic pulmonary heart disease: chronic asthma, complicated chronic bronchitis, emphysema, etc. [/double_paragraph] [/row]
Acute heart failure – this is a sudden affection of the ability of the heart to pump blood. Symptoms of this form of congestive heart failure are similar to those of chronic heart failure, but they tend to be more severe and more apt to lead to complications. Acute heart failure is a common reason for hospitalization in emergency in the elderly; it often requires aggressive and urgent therapeutic decisions. Despite advances in medical science, the mortality rate after an acute heart failure remains high.
Although causative factors leading to chronic heart failure can also be responsible for the disease, acute heart failure is mostly the result of:
- chronic coronary disease
- viral infection of the myocardium
- severe or chronic infection
- sudden allergic reaction
- presence of blood clots in the lungs
- use of certain medications such as pioglitazone (Actos) and rosiglitazone (Avandia).
Heart Failure Symptoms
The role of the heart is to pump blood and deliver oxygen and important nutrients to the entire body. When you have congestive heart failure, all organs in your body can be affected, leading to development of various symptoms. However, the onset of heart failure is often asymptomatic; the disease progresses, but without producing any apparent symptoms. As the failure progresses and gradually damages the heart tissue, symptoms begin to emerge./heart-failure-symptoms-5ad8b9bfae9ab80038133c25.png)
To describe the severity of heart failure, progression of symptoms is often classified into 4 classes: I, II, III or IV:
Class I – during this stage, the disease is completely asymptomatic; you feel no shortness of breath, or abnormal fatigue during exercise; however, the damage continues in your heart muscle.
Class II – the heart failure presents mild symptoms that may go unnoticed or taken for other medical conditions; a Class II heart failure can be associated with breathlessness and fatigue during or even after moderate activity.
Class III – Class III marks an important stage in the disease. Symptoms pass from moderate to severe; you may experience breathlessness even at rest; you may experience fatigue even during routine activities such as walking in your house, cooking or climbing stairs.
Class IV – this last stage of the disease indicates a severe and life threatening heart failure. you can feel exhausted, tired or breathless during any insignificant effort. Shortness of breath and fatigue can happen even when you sit or lie quietly in bed. You need medical treatment urgently to prevent complications.
In addition to fatigue and shortness of breath, heart failure is often accompanied by symptoms and signs:
[row][double_paragraph]- diarrhea
- shortness of breath
- decreased appetite
- abdominal fullness
- abnormal or rapid heartbeat
- nausea and vomiting
- decreased production of urine (Oliguria)
- large quantities of gastric/intestinal gas
- difficulty concentrating or decreased alertness
- swelling (edema) in the legs, ankles and feet
- persistent cough or wheezing, which often associated with white or pink blood-tinged phlegm
- pleural fluid in the peritoneal cavity (mostly acute heart failure)
- enlarged Jugular Vein (vein in the neck) either at rest or after applying pressure.[/double_paragraph] [/row]
Diagnosis
Even if you experience symptoms typical of a congestive heart failure, only your doctor can confirm that you have the disease. Heart problem is a matter of extreme importance; do not rely on friends, family or any unprofessional information to conclude or exclude you have heart failure; a diagnosis is crucial. Your heart failure diagnosis will be based on an interrogation between you and your cardiologist, physical exam and several other medical procedures. In general, your cardiologist will recommend all or some of the following tests:
Physical exam – a clinical exam is an important part of heart failure diagnosis. It allows your doctor to get an idea of the functioning of your cardio-vascular system. During the examination, you will be asked a series of question concerning your medical history. In addition, your physician will search for signs indicating cardiovascular problems especially congestive heart failure: high blood pressure, heart murmur, shortness of breath, abdominal fullness, abnormal or rapid heartbeat, etc. However, spite all evidence, a physical exam is not sufficient to confirm a heart failure; other tests are needed.
Blood test – a sample of your blood may be taken to search for biological signs of kidney and thyroid problems which can be associated with congenital heart failure. The test can reveal a high rate of brain natriuretic peptide (B-type natriuretic peptide or BNP), a cardiac marker that is often higher in patients with acute congestive heart failure. An increased rate is a sign indicating severe systolic heart failure.
In addition, the blood test is also conducted to find an elevated troponin, protein complex (or multiprotein complex) of cardiac muscle and those of the skeleton. High rate can confirm the diagnosis of an unstable angina pectoris, heart attack (myocardial infarction), heart failure and/or other heart problems.
Chest X-ray – this exam is a common imaging technique allowing your doctor to evaluate your lungs, heart and chest wall. An X-ray not only helps visualize the size and shape of your heart but also helps discover heart failure and other diseases of the heart muscle.
Electrocardiogram (ECG) – electrocardiography is a painless technique often performed to detect a congestive heart failure. It allows your cardiologist to measure and record changes in electrical activity of heart cells. During the procedure, you will be asked to lie flat on a bed or table while electrical sensing devices (EKG leads) are attached to your body, precisely on the front of your chest. To facilitate the transmission of the electrical impulses of your heart, a small amount of gel can be applied to the skin of your chest. An ECG can allow your cardiologist to detect:
- rhythm of the heart
- abnormal electric activity
- presence of injury or damage to the various parts of the cardiac muscle
- hypertrophy of the heart muscle (enlarged heart)
- the position of the heart in the chest cavity
- obstruction of blood flow to the heart muscle.
Echocardiogram – An echocardiogram is the use of sound waves (ultrasound) to create picture of the heart. It allows your physician to visualize and record the shape and texture of the heart muscle. In addition, an echocardiogram can help your physician discover impaired blood flow to the heart muscle, movement of the valves and the volume and function of cardiac chambers.
Coronary catheterization (angiogram) – this cardiology diagnostic test consists of using a thin catheter along with computerized tomography to visualize your heart muscle, especially the blood filled chambers. With a coronary catheterization, your cardiologist can detect internal functioning and pathologies in the heart muscle and in certain blood vessels like the aorta. In addition, this test is also used to detect narrowing or blockage of the carotid arteries that carries blood from the heart to the brain.
Implantable ECG recorder: takes about 25 minutes, this surgical procedure is performed under local anesthesia. During the operation, the specialist places a small device under your skin to continuously record your heart’s electrical activities. Depending on the condition of your heart, this device can remain under your skin for more than a year.
Heart Failure Treatment
There are today several therapeutic approaches to treat congestive heart failure. Heart failure treatments aim at slowing or stopping the progression of the disease, and reducing symptoms to improve the quality of your life. It is important to have, along with the medical treatment, a healthy lifestyle, eat a healthy heart diet, and exercise moderately and regularly (get approval of your cardiologist before doing any exercise if you already are diagnosed with heart disease). Treatments of congestive heart failure can include medications, implantation devices and surgery. Early diagnosis and treatment can significantly reduce the symptoms of the disease and allows you to resume an active life.
Lifestyle changes – changes in lifestyle consisting of implementation of all measures allowing you to combat and prevent symptoms and complications of the disease. Therefore, during treatment and the rest of your life, it is important to:
- stop smoking
- treat or prevent obesity
- avoid a stressful life
- sleep 7 to 8 hours per day
- avoid heavy alcohol consumption
- reduce your salt intake
- perform moderate physical activity regularly
- take adequate time to rest
- adopt a heart healthy diet (see heart diet).
Medications
Angiotensin-converting enzyme (ACE) Inhibitors – ACEs are a class of medication often used to treat hypertension and chronic heart failure. They can be very effective in treatment of congestive heart failure, especially systolic dysfunction. In most cases, ACE inhibitors are given in high doses to reduce the symptoms. However, in cases of kidney problems or a dangerous decreased blood pressure, lower doses may be recommended.
In addition, ACE inhibitors are used in the treatment of asymptomatic backward heart failure of the left ventricle to slow the progression of the disease and also reduce the risk of myocardial infarction (heart attack) or/and sudden death. It is recommended to have regular monitoring of renal functions before treatment, one to two weeks after the beginning of the treatment, and every three to six months during the treatment. During treatment, you can experience:
- cough
- hypotension
- kidney failure
- hyperkalemia
- loss of consciousness
- and more…
Angiotensin Receptor Blockers (ARBs) – this class of drug is often used as an alternative to inhibitors of angiotensin–converting enzyme (ACE) in patients who cannot tolerate them; ARBs causes fewer side effects, and tend to be tolerated by most patients. That is, if you develop severe and persistent side effects while taking ACE inhibitors, your cardiologist may recommend you to stop taking ACE inhibitors to take angiotensin receptor blockers. Depending on the severity of the side effects, the ARBs can be associated with other medications to reduce your risk of death or relapse of the heart failure. Most common of the ARBs are losartan (Cozaar) and valsartan (Diovan).
Diuretics – diuretics such as bumetanide (Bumex) and furosemide (Lasix) prevent fluids from accumulating in your body. Loop diuretics and thiazides (another form of diuretics) are used in cases of fluid overload that lead to peripheral edema or pulmonary edema. As far as possible, diuretics should be prescribed to be taken in combination with ACE inhibitors and beta blockers.
If you taking diuretic medications, consider talking to your health care provider about potassium and magnesium; diuretic drugs tends to lower these minerals in your blood.
Beta blockers – this class of medication is used to treat a variety of heart diseases. Beta blockers such as nebivolol, carvedilol (Coreg), metoprolol (Lopressor) and bisoprolol (Zebeta) are used to treat acute and chronic heart failure. Along with a healthy diet, these drugs can slow the heart rate, lower blood pressure and reduce symptoms of heart failure. Provided there are no contraindications, Beta blocker drugs should be taken in combination with diuretics and ACE inhibitors to more effectively reduce the progression of the heart failure.
Aldosterone antagonists – this class of drugs plays an important role in the homeostasis of sodium and water, notably in case of heart failure or hypertension. They act by preventing and reversing damage of heart failure and therefore help improve lives of patients living with the disease. However, aldosterone antagonists can lead to hyperkalemia (excess potassium in the blood plasma) if they are not used in association with diuretics. The most common of aldosterone antagonists include spironolactone (Aldactone) and eplerenone (Inspra).
Surgical treatment
Implantable cardioverter-defibrillator (ICD) – an implantable cardioverter-defibrillator is a type of pacemaker use to treat patients with serious heart problem to detect and correct instantly abnormal electrical activities in the heart by delivering a jolt of electricity. ICD is indicated for the prevention of sudden death, mainly in heart disease patients with mechanical malfunction of the left ventricle.
Cardiac resynchronization therapy (CRT) – also known as biventricular pacing, CRT is the implantation of a pacemaker to send timed electrical impulses to the right and left ventricles. It increases the force of contraction of the heart by re-coordinating the action of the right and left ventricles. CRT is a recent therapeutic method to treat patients with advanced heart failure resulting from systolic dysfunction refractory to medical treatment. This therapy is used in cases of heart failure with moderate to severe persistent symptoms despite use of appropriate medications.
Ventricular Assist Device (VAD) – This therapy consist of using a medical circulatory device to partially or completely replace the function of a failing heart. Some VADs are intended for short term use, typically for patients recovering from a heart attack or heart surgery. In case of congestive heart failure, the device may be recommended for long term or lifetime use.
Heart Failure Prevention
 Heart failure prevention has many facets. You must adopt a healthy lifestyle, detect and treat hypertension coronary disease and major factors that can lead to congestive heart failure. If you’re at risk, even when you do not feel any symptom, it is important to regularly see your cardiologist. To prevent all types of heart disease including congestive heart failure, it is necessary to:
Heart failure prevention has many facets. You must adopt a healthy lifestyle, detect and treat hypertension coronary disease and major factors that can lead to congestive heart failure. If you’re at risk, even when you do not feel any symptom, it is important to regularly see your cardiologist. To prevent all types of heart disease including congestive heart failure, it is necessary to:
- not smoke
- avoid stress
- exercise
- maintain a healthy weight
- control your blood pressure
- avoid heavy alcohol consumption
- maintain normal cholesterol levels
- adopt a heart-healthy diet – eating plenty of fruits and vegetables; they are rich in nutrients that help the heart and blood vessels to accomplish their function. Being rich in antioxidants and fiber, fruits and vegetables prevent the oxidation of cholesterol, which contributes in the development of blood clot. A diet consisting mainly of fruits and vegetables prevents the development of many cardiovascular diseases.
References :
1 – (fr) Traitement de l’insuffisance cardiaque aiguë : J.-L. Gérard, J.L. Hanouz ; Département d’anesthésie-réanimation chirurgicale et de médecine d’urgence, CHU Côte-de-Nacre, 14033 Caen cedex, France
2 – National Heart, Lung, and Blood Institute: Cardiac failure, CHF, Left-sided heart failure, Right-sided heart failure
3 – Schaufelberg M, Swedberg K, Koster M et als. Decreasing one year mortality and hospitalisation rates for heart failure in Sweden. Data from the Swedish Hospital Discharge Registry, Eur Heart J, 2004;25:300–307
4 – Zannad F, Braincon S, Juillère Y et als. Incidence, clinical and etiologic features, and outcomes of advanced chronic heart failure: the EPICAL Study. Epidemiologie de l’Insuffisance Cardiaque Avancée en Lorraine, J Am Coll Cardiol, 1999; 33:734-42
5 – On parle en toute rigueur de volume télésystolique et de volume télédiastolique, le terme “télé” signifiant “fin de “. Les volumes ainsi définis correspondent aux valeurs minimales et maximales des volumes ventriculaires.
6 – Maisel AS, Krishnaswamy P, Nowak RM, et als. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure, N Engl J Med, 2002;347:161-167
7 – Sugiura T, Takase H, Toriyama T, Goto T, Ueda R, Dohi Y, Circulating levels of myocardial proteins predict future deterioration of congestive heart failure, J Card Fail, 2005;11:504-509
8 – Peacock WF, De Marco T, Fonarow GC et Als. Cardiac troponin and outcome in acute heart failure, N Eng J Med, 2008;358:2117-2126
9 – Tang W, Tong W, Measuring impedance in congestive heart failure: Current options and clinical applications, Am Heart J, 2009;157:402-411
10 – Packer M, Abraham WT, Mehra MR et als. Utility of impedance cardiography for the identification of short-term risk of clinical decompensation in stable patients with chronic heart failure, J Am Coll Cardiol, 2006;47:2245–2252
11- Jessup M, MD, Abraham WT, Casey RE et Als, 2009 Focused Update: ACCF/AHA Guidelines for the Diagnosis and Management of Heart Failure in Adults, Circulation, 2009;119:1977-2016
12 – Dickstein K, Cohen-Solal A, Filippatos G et als, Task Force for Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of European Society of Cardiology; ESC Committee for Practice Guidelines, ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008, Eur Heart J, 2008;29:2388-2442
13 – Swedberg K, Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005) The Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology, European Heart Journal, 2005;26:1115-1140
14 – O’Connor CM, Whellan DJ, Lee KL et Als. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial, JAMA, 2009;301:1439-1450
15 – Flynn KE, Piña IL, Whellan DJ, Effects of exercise training on health status in patients with chronic heart failure: HF-ACTION randomized controlled trial , JAMA, 2009;301:1439-1450
16 – Flather M, Yusuf S, Kober L et als. Long-term ACE-inhibitor therapy in patients with heart failure or left-ventricular dysfunction: a systematic overview of data from individual patients. ACE-Inhibitor Myocardial Infarction Collaborative Group, Lancet, 2000;355:1575–1581.
17 – Les guides ALD de l’Haute Autorité de Santé: Insuffisance cardiaque systolique symptomatique chronique. guide ALD n°5; 22/5/2007
18 – The CONSENSUS Trial Study Group, Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS), N Engl J Med, 1987;316:1429–1435.
19 – Pfeffer MA, Braunwald E, Moye LA et als. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial, N Engl J Med 1992;327:669–677
20 – Revue Médicale Suisse : Le renouveau des antagonistes de l’aldostérone ; B. Waeber. Revue Médicale Suisse N° 78 publiée le 13/09/2006
21 – http://www.sciencedaily.com/releases/2003/09/030909065952.htm
22 – Tracy, CM; et al. (Oct 2, 2012). “2012 ACCF/AHA/HRS focused update of the 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. [corrected].” (PDF). Circulation 126 (14): 1784–1800. doi:10.1161/CIR.0b013e3182618569. PMID 22965336. Retrieved Apr 29, 2015.
23 – Kuck, K.-H.; et al. (Jan 2014). “New devices in heart failure: an European Heart Rhythm Association report: developed by the European Heart Rhythm Association; endorsed by the Heart Failure Association” (PDF). Europace 16 (1): 109–128. doi:10.1093/europace/eut311. PMID 24265466. Retrieved Oct 13, 2014.
24 – Dickstein K, Cohen-Solal A, Filippatos G, et al. (October 2008). “ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM)”. Eur. Heart J. 29 (19): 2388–442. doi:10.1093/eurheartj/ehn309. PMID 18799522.
25 – “congestive heart failure” at Dorland’s Medical Dictionary
26 – “Ejection Fraction Heart Failure Measurement”. American Heart Association. Feb 11, 2014. Retrieved 7 June 2014.