Table of Contents
Pulmonary Hypertension
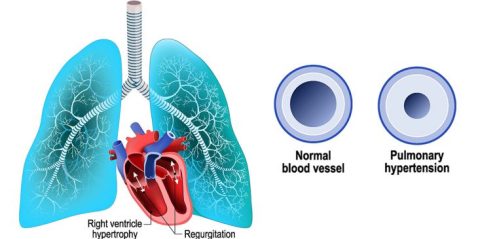
Pulmonary hypertension is a form of high blood pressure localized only in the arteries of the lungs and the left side of the heart. Usually, pulmonary hypertension occurs when vessels supplying blood to the lungs are narrowed or blocked. The obstruction impairs the blood circulation, increases blood pressure in the pulmonary arteries and disrupts the functioning of the heart.
Depending on the cause, pulmonary hypertension can be a life threatening disease with risk of right heart failure and even death in absence of effective treatments. However, thanks to progress of medical science, now days, there are new curative treatments for pulmonary hypertension; the chances of survival are higher than in the past.
Unlike high blood pressure, pulmonary hypertension is a rare disease with an estimate of 500 to 1,000 new cases each year in the US, according to American Heart Association. Although the disease affects both sexes and people of any age, women between ages 20 and 40 are more victims of pulmonary hypertension, according to the same research.
Pulmonary Hypertension Causes
Pulmonary hypertension occurs when blood flow is slowed or obstructed in the arteries that supply blood to the lungs. Normally, the average blood pressure in the pulmonary artery is 14 mmHg at rest. When you have pulmonary hypertension, the pressure may rise above 25 mmHg at rest and above 30 mmHg during physical activities.
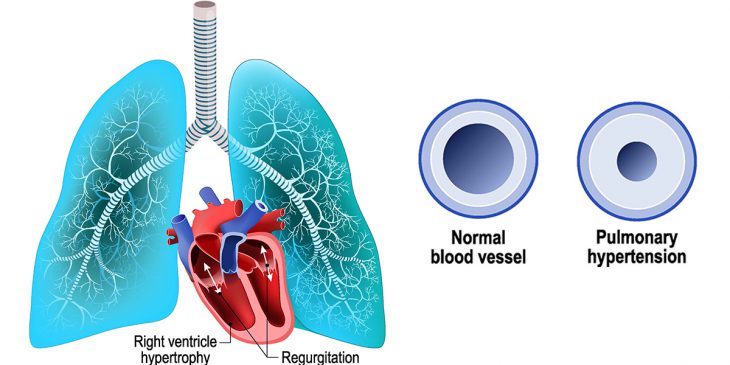 Passing of blood through your lungs is very important. That is in the lungs that oxygen and carbon dioxide are exchanged; the blood is gotten rid of carbon dioxide and enriched with oxygen. That is, when the pulmonary arteries and capillaries are narrowed, blocked or destroyed, the heart is depressed of oxygen necessary needed to function properly.
Passing of blood through your lungs is very important. That is in the lungs that oxygen and carbon dioxide are exchanged; the blood is gotten rid of carbon dioxide and enriched with oxygen. That is, when the pulmonary arteries and capillaries are narrowed, blocked or destroyed, the heart is depressed of oxygen necessary needed to function properly.
When the cause is known, the development of pulmonary hypertension is often due to heart or/and lung diseases. However, most of the times, the cause is unknown. In addition, the causes of pulmonary hypertension tend to vary depending on its type; primary pulmonary hypertension and secondary pulmonary hypertension.
There are many types of pulmonary hypertension; the most common include:
Primary pulmonary hypertension – also known as idiopathic pulmonary arterial hypertension, primary pulmonary hypertension is not originated from another disease (heart or/and lung disease); the disease develops without apparent reason.
Secondary pulmonary hypertension – this form of pulmonary hypertension is directly associated with another medical condition. Some medical problems suspected in the development of secondary pulmonary hypertension include:
- HIV / AIDS
- sleep apnea
- infections
- pulmonary fibrosis
- sickle cell anemia
- cystic Fibrosis
- family history of pulmonary hypertension – very rare
- limited scleroderma (CREST syndrome)
- left-sided heart failure
- congenital heart disease
- liver diseases such as cirrhosis
- pulmonary embolism – sudden blockage in a lung artery
- chronic obstructive pulmonary disease (COPD), emphysema for instance
- use of certain drugs, amphetamine for instance
- Connective tissue diseases such as systemic lupus, scleroderma, polymyositis (inflammation and weakness of the muscle fibers) and dermatomyositis (inflammation and rash of the skin).
Pulmonary Hypertension Symptoms
:max_bytes(150000):strip_icc()/los-pulmones-y-sus-funciones-56a299423df78cf77277ef78.jpg) You may have pulmonary hypertension for years without noticing any symptom. The disease continues damaging your organs silently. In fact, most of the times, when you finally feel signs or symptoms, the problem is already complicated. In general, as the disease worsens, you may experience the following pulmonary hypertension symptoms:
You may have pulmonary hypertension for years without noticing any symptom. The disease continues damaging your organs silently. In fact, most of the times, when you finally feel signs or symptoms, the problem is already complicated. In general, as the disease worsens, you may experience the following pulmonary hypertension symptoms:
- fatigue
- shortness of breath
- heart palpitations
- chest pain
- bluish color of your lips and skin (cyanosis)
- dizziness
- unconsciousness (fainting)
- Swelling of your ankles, legs and possibly your abdomen.
Complications
High blood pressure has an impact mainly on the right ventricle. Untreated or poorly treated pulmonary hypertension can lead to right ventricular hypertrophy, and then ventricular failure, which can lead to breathlessness on exertion, edema of lower limbs, and increased volume of the liver. If the condition persists, the pulmonary hypertension can lead to irreversible heart failure and even sudden cardiac arrest during exertion.
Diagnosis
The diagnosis aims at not only discovering the pulmonary hypertension but also its severity; therefore, your doctor will perform many diagnostic procedures.
Physical examination – at first, your physician will do a physical exam to look for signs related to pulmonary hypertension: high blood pressure, swelling of the ankles and feet, abnormal heart sounds, affection of the fingers and fingernails, and abdominal swelling due to the accumulation of fluid. During the physical exam, you may be asked questions about your medical history in a way to determine if you have diseases that can lead to pulmonary hypertension.
Six-Minute Walking Test – to measure the severity of the disease, your physician will ask you to do a “Six-Minute Walking Test”. During the test, you will be asked to walk back and forth in a flat indoor surface (a hallway for instance) for six minutes. Depending on the reaction of your body during the test, you may be asked to slow down, stop, or rest. Borg scale is used to determine the severity of your respiratory problem. The results of the test will help your physician to determine an exercise program designed to meet your needs.
In general, the development of hypertension is grouped into four classes according to the limitation of physical activity.
- Class I: You have pulmonary hypertension, but you are able to do normal physical activities without any ambiguity.
- Class II: in this stage of pulmonary hypertension, usually physical activities are somewhat limited by symptoms such as dyspnea, fatigue, and chest pain or fainting.
- Class III: in this advanced stage of pulmonary hypertension, your limitation to do certain physical activities is remarkable, but the disease is asymptomatic at rest. Symptoms such as fatigue, chest pain can manifest during minor efforts or activities of daily life.
- Class IV: a class IV pulmonary hypertension is a serious conditions; inability to do your daily routine or exercise is very remarkable. Symptoms of right heart failure such as dyspnea, fatigue, and breathlessness may be present even at rest. You are unable to make even the routine activities of life.
The Six-Minute Walking Test, however, is not enough to confirm the diagnosis. Other specific exams should be performed to rule out other diseases that have similar symptoms to pulmonary hypertension.
Blood test – a blood test is important to detect the presence of autoantibodies, which may indicate an autoimmune disease. In addition, the blood test allows your health care provider to confirm or rule out certain pulmonary hypertension related diseases such as AIDS / HIV and liver disease.
Another importance of the blood test is to determine the endothelin level. In general, high endothelin levels are found in plasma and lung tissue of patients with pulmonary hypertension. This rate indicates not only the presence of disease but also its severity.
Electrocardiogram (ECG) – the ECG is a medical technique performed to record electrical stimulation that the heart receives to be able to contract. Using this exam, your physician may detect abnormality or hypertrophy of the right ventricular and/or atrium. The rhythm is usually normal, although arrhythmias are possible. However, a normal ECG does not mean the absence of pulmonary hypertension; more exams are needed.
Chest X-ray – a chest x-ray is important diagnostic procedure allowing your physician to detect abnormalities in the lungs. It may show an increase in the size of the cardiac silhouette and the volume of the pulmonary arteries. In addition, the x-ray can also allow your physician presence of blockage in the pulmonary arteries. A chest-ray, however, is unreliable; it can be normal although you have pulmonary hypertension.
Pulmonary artery catheterization (PAC) – also known as right heart catheterization (CCD) or Swan-Ganz catheterization, PAC is often regarded as an irreplaceable technique to monitor pulmonary hypertension. Unlike the chest-ray, it helps your physician to detect and establish with certainty the existence of pulmonary hypertension. During the procedure, the specialist inserts a long catheter, under radiological control, into a pulmonary artery. The definition of pulmonary hypertension is based on the finding of abnormally high numbers of pulmonary pressures.
Cardiac Ultrasound – an ultrasound is a painless technique used to image the heart muscle accurately. During the procedure, a probe is applied on your chest, and signals are sent by the different structures of the heart, then recovered and decoded on a television screen, where your doctor can observe the movements of the heart. The echocardiogram allows the diagnosis and assesses the severity of the disease. The right cavities (right ventricle and right atrium) are typically dilated in a pulmonary hypertension diagnosis.
Thoracic CT – your doctor can recommend a computed tomography scan of the chest and upper abdomen to detect anomalies in the organs and vessels of your chest: lungs, heart and great vessels, etc. During the exam, two sets of images are always obtained: some without a medical contrast medium and some with a radiocontrast agent. Your doctor will recommend a chest CT scan to identify an anomaly that was discovered in the chest radiograph or to monitor the evolution of a pulmonary hypertension during the treatment.
Lung perfusion scan – this test is performed to obtain images of the lungs and measure breathing and circulation in all areas of the lung after having injected, intravenously, radioactive biodegradable particles of few tens of microns in diameter. Radioactive particles are temporarily blocked in pre-pulmonary capillary open to blood flow. The lung areas poorly or not perfused, however, are not radioactive.
A lung perfusion scan also allows your doctor to detect a pulmonary embolism or respiratory failure. However, a normal scan does not eliminate the diagnosis of pulmonary embolism (blockage of the artery of the lung).
Pulmonary function tests – the pulmonary function tests (PFT) include all explorations allowing your doctor to evaluate your respiratory capacity. In addition, the PFT allows your physician to detect chronic pulmonary obstructive and all other pulmonary pathologies. These exams are not only important in detecting pulmonary hypertension, but also in following the evolution of the disease during treatment.
Open lung biopsy – during the lung biopsy your physician removes from your lungs a small sample of tissue is to check for cancer cells, lung infection or disease. This test is not without risk, but it is sometimes necessary if the other diagnostic procedure do not give conclusive results. In general, an open lung biopsy is done in a hospital operating room under general anesthesia.
Pulmonary Hypertension Treatment
The treatment recommended by your doctor for the pulmonary hypertension varies depending on your age, the class of the disease (see diagnosis for pulmonary hypertension class) and the severity of the symptoms. In case it is not primary pulmonary hypertension, that is, the diagnosis has revealed the cause, the treatment of the cause is very important. In general, treatment of pulmonary hypertension involves taking drugs, oxygen therapy or/and sometimes surgery.
Medications
Several drugs are used to treat pulmonary hypertension. Some are taken orally, others are administered by injection. However, most of those drugs reduce the symptoms at the beginning of the treatment, but they are not effective in long-term. The most common drugs used to treat pulmonary hypertension include:
Anticoagulants – these medications have the property of inhibiting the natural blood clotting, and preventing the risk of blood clot within the pulmonary arteries. Anticoagulant drugs may be taken by injection or orally. In addition to pulmonary hypertension, anticoagulant drugs are also used in the treatment of heart attack, stroke, and certain cardiac arrhythmias such as atrial fibrillation.
Blood Vessel Dilators – also called vasodilators, blood vessel dilators are drugs intended to increase the size of the pulmonary vessels to facilitate the blood flow. The injection is made through the insertion of a catheter and a device that you carry with you always. Epoprostenol (Flolan) is one of the most popular vasodilator used in the treatment of pulmonary hypertension. However, its effectiveness does not last, and it often causes a variety of side effects:
[row][double_paragraph]
- Chills
- Fever
- Sore throat
- Nausea
- Headache
- Vomiting
- Loss of appetite
- Diarrhea
- Dizziness
[/double_paragraph][double_paragraph]
- Jaw pain
- Flushing
- Sweating
- Drowsiness
- Muscle aches
- Stomach pain
- Chest pain
- Vision problems.
[/double_paragraph] [/row]
Calcium antagonists (calcium channel blockers) – in some patients suffering from pulmonary hypertension, calcium channel blockers are sometimes used to effectively decrease blood pressure. These drugs act by inhibiting the transfer membrane of calcium in the cardiac muscle cells and decrease the oxygen consumption of the myocardium. This class of drugs is widely used in the treatment of pulmonary hypertension and coronary artery disease.
Inhibitors of endothelin – this class has been introduced recently in the treatment of pulmonary hypertension, inhibitors of endothelin appears very promising in the fight against pulmonary hypertension.
Endothelin receptor antagonists – this class of medications has been introduced recently in the treatment of pulmonary hypertension. They act by reversing the effect of endothelin, a group of vasoconstrictive peptides produced by endothelial cells that cause the walls of blood vessels to narrow. Bosentan (Tracleer) is one of the endothelin receptor antagonists used to treat pulmonary hypertension.
In some patients, Tracleer reduce the symptoms of the disease; however, it can cause severe liver problems and it is not recommended for pregnant women or those who are breast-feeding.
Sildenafil – sildenafil is a drug belonging to the class phosphodiesterase type 5 inhibitor (PDE5 inhibitor). It works by blocking the action of PDE5 inhibitor, an enzyme presents in smooth muscle cells lining the blood vessels supplying the tissue of the penis and the arterial wall within the lungs. Therefore, sildenafil is used to treat erectile dysfunction and pulmonary hypertension who had not responded adequately to other treatments. PDE5 inhibitors, when used to treat pulmonary hypertension, lower blood pressure by widening blood vessels in the lungs.
Diuretics – diuretics such as bumetanide (Bumex) and furosemide (Lasix) prevent accumulation of fluids in your body. If your doctor thinks it is necessary, he can prescribe you loop diuretics and thiazides along with other medication to your pulmonary hypertension. As far as possible, diuretics should be taken in combination with ACE inhibitors and beta blockers.
In addition, if you consider taking diuretics, it is important to talk to your health care provider about potassium and magnesium; diuretic medications can lower those minerals in your blood.
Oxygen Therapy
If the oxygen level in blood is low or you have chronic respiratory failure characterized by fatigue, breathlessness and fainting, your doctor may prescribe your supplemental oxygen. In addition, you can be recommended oxygen therapy if you have sleep apnea. Depending on the severity of the pulmonary hypertension, you may require constant oxygen therapy.
Surgical Treatment
Pulmonary hypertension can be treated with a lung transplant when other methods have failed. Surgery is always the last attempt. Your surgeon will remove your lung or heart-lung block to replace it with another one. However, lung transplantation is not always recommended; there is no guarantee of success. Even if the operation would be performed successfully, you would have to take immunosuppressants for life to help reduce the chance of rejection. Taking immunosuppressant drugs puts you at high risk of infectious diseases and a variety of life threatening medical conditions including cancer. Therefore, it is better to talk to your doctor to try all means to prevent or slow the deterioration of your lung function rather than perform a lung transplant; it is very risky.
Pulmonary Hypertension Prevention
There is no specific method to prevent pulmonary hypertension; however, to reduce your risk of having pulmonary hypertension and all other cardiovascular diseases, you need to:
- exercise regularly
- lose weight (if you are obese or overweight)
- Stop smoking (including second hand smoke).
In addition, you need to avoid fast foods and adopt a healthy diet.
- Increase your intake of antioxidants
- Avoid saturated acids, mainly from animal fats, pastries, margarine, etc.
- Increase your intake of carbohydrates and fiber; they play an important role in increasing the levels of good cholesterol
- Reduce bad cholesterol: egg yolk, organ meats (brain, kidney, liver), nuts, almonds, lobster, shellfish, fish eggs, etc.
- Consuming polyunsaturated fatty acids such as omega-6 (sunflower oil) omega 3 (flax seed oil, fish oil); they lower the bad LDL cholesterol and prevent the formation of a blood clot.
- Eat plenty fruits (2 to 3 per day), vegetables (3 to 4 servings per day), polyphenols (moderate consumption of wine and green tea) and phyto-oestrogens: soy, green tea, chickpeas, lentils, beans, grains, carrots, fennel, onions, garlic, etc.
1 – americanheart.org, Primary or Unexplained Pulmonary Hypertension: retrieved August 31, 2009
2- Rich S, Rubin LJ, Abenhail L et al. (1998). Executive summary from the World Symposium on Primary Pulmonary Hypertension (Evian, France, September 6–10, 1998). Geneva: The World Health Organization.
3 – http://web.archive.org/web/20020408173726/http://www.who.int/ncd/cvd/pph.html.
Gladwin MT, Sachdev V, Jison ML, et al. (2004). “Pulmonary hypertension as a risk factor for death in patients with sickle cell disease“. N. Engl. J. Med. 350 (9): 886–95. doi:10.1056/NEJMoa035477. PMID 14985486. http://content.nejm.org/cgi/content/full/350/9/886.
4 – Cool CD, Rai PR, Yeager ME, et al. (2003). “Expression of human herpesvirus 8 in primary pulmonary hypertension“. N. Engl. J. Med. 349 (12): 1113–22. doi:10.1056/NEJMoa035115. PMID 13679525. http://content.nejm.org/cgi/content/full/349/12/1113.
5 – Rudarakanchana, N; Trembath RC, Morrell NW (November 2001). “New insights into the pathogenesis and treatment of primary pulmonary hypertension“. Thorax 56 (11): 888–890. doi:10.1136/thorax.56.11.888. PMID 11641516.
6 – Torres F (2007). “Systematic review of randomised, double-blind clinical trials of oral agents conducted in patients with pulmonary arterial hypertension“. Int. J. Clin. Pract. 61 (10): 1756–65. doi:10.1111/j.1742-1241.2007.01545.x. PMID 17877662. http://www.blackwell-synergy.com/doi/full/10.1111/j.1742-1241.2007.01545.x.
7- “UPDATE 1-Encysive gets Canadian approval for hypertension drug“. Reuters. 2008-05-30. http://www.reuters.com/article/governmentFilingsNews/idUSBNG28335020070530. Retrieved 2007-07-08.
8 – Gilead Sciences (2007-06-15). “U.S. Food and Drug Administration Approves Gilead’s Letairis Treatment of Pulmonary Arterial Hypertension“. Press release. http://www.gilead.com/wt/sec/pr_1016053. Retrieved 2007-06-16.
9 –2006 OPTN/SRTR Annual Report“. US Scientific Registry of Transplant Recipients. 2006-05-01. http://www.ustransplant.org/annual_reports/current/113_surv-new_dh.htm. Retrieved 2007-03-28.
10 – McLaughlin VV, Sitbon O, Badesch DB, et al. (2005). “Survival with first-line bosentan in patients with primary pulmonary hypertension“. Eur. Respir. J. 25 (2): 244–9. doi:10.1183/09031936.05.00054804. PMID 1568428
11 – Members, Authors/Task Force; Galiè, Nazzareno; Hoeper, Marius M.; Humbert, Marc; Torbicki, Adam; Vachiery, Jean-Luc; Barbera, Joan Albert; Beghetti, Maurice; Corris, Paul (2009-10-01). “Guidelines for the diagnosis and treatment of pulmonary hypertension”. European Heart Journal 30 (20): 2493–2537. doi:10.1093/eurheartj/ehp297. ISSN 0195-668X. PMID 19713419.
12 – “How Is Pulmonary Hypertension Diagnosed? – NHLBI, NIH”. www.nhlbi.nih.gov. Retrieved 2016-05-20.
13 – “Guidelines:Six-minute Walk Test” (PDF). American Thoracic Society. 2002. Retrieved 2016-05-20.
14 – Bossone, Eduardo (2011). “Echocardiography in Pulmonary Arterial Hypertension:From Diagnosis to Prognosis” (PDF). Journal of the American Society of Cardiology. Retrieved 2016-05-20.
15 – “Swan-Ganz – right heart catheterization: MedlinePlus Medical Encyclopedia”. www.nlm.nih.gov . Retrieved 2016-05-20.
16 – Taleb M, Khuder S, Tinkel J, Khouri SJ (2013). “The diagnostic accuracy of Doppler echocardiography in assessment of pulmonary artery systolic pressure: a meta-analysis.”. Echocardiography 30 (3): 258–65. doi:10.1111/echo.12061. PMID 23227919
17 – American College of Chest Physicians; American Thoracic Society (September 2013), “Five Things Physicians and Patients Should Question”, Choosing Wisely: an initiative of the ABIM Foundation (American College of Chest Physicians and American Thoracic Society), retrieved May 27, 2016
18 – “Pulmonary Hypertension. About Pulmonary Hypertension | Patient”. Patient. Retrieved May 27, 2016.
19 – McLaughlin VV, Sitbon O, Badesch DB, et al. (2005). “Survival with first-line bosentan in patients with primary pulmonary hypertension”. Eur. Respir. J. 25 (2): 244–9. doi:10.1183/09031936.05.00054804. PMID 15684287
20 – British Journal of Anaesthesia: “Primary pulmonary hypertension in pregnancy; a role for novel vasodilators” March 19, 2016
21 – “Primary Pulmonary Hypertension: Practice Essentials, Background, Pathophysiology”.
22 – York, Michael; Farber, Harrison W. (November 2011). “Pulmonary Hypertension: Screening and Evaluation in Scleroderma”. Current Opinion in Rheumatology 23 (6): 536–544. doi:10.1097/BOR.0b013e32834ba6a7. Retrieved May 27, 2016