Table of Contents
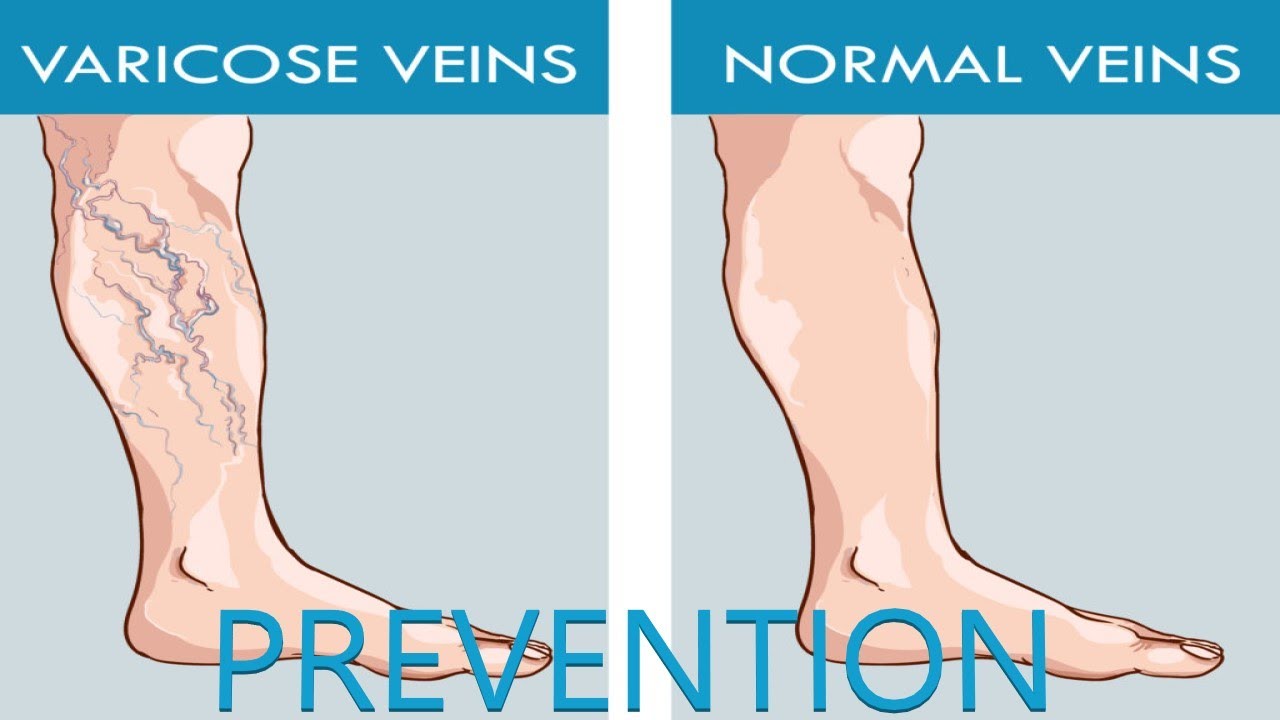
 Varicose veins are permanent dilations of the veins, usually on the legs and feet. Varicose veins are usually sinuous, they have many curves. Being full with blood, they can cause pain, discomfort, aching and heavy legs which often become worse at night and after exercise.
Varicose veins are permanent dilations of the veins, usually on the legs and feet. Varicose veins are usually sinuous, they have many curves. Being full with blood, they can cause pain, discomfort, aching and heavy legs which often become worse at night and after exercise.
Varicose veins can present some cosmetic problems. For women, having varicose veins can be embarrassing. In addition to cosmetic effects, the disorder can lead to major complications due to poor circulation of blood through the affected limb.
Although varicose veins can affect both men and women, the affection is more common in women than in men. Other factors that are shown to be associated with the disease include heredity, pregnancy, obesity, menopause and aging.
Varicose Veins Causes
The function of your veins is to deliver blood to your heart from the outer parts of your body. To achieve this crucial task, they have a multitude of valves that open in one direction, forcing the oxygen-poor blood to flow one way into the heart. When the walls of the veins lose their elasticity and their tone, the veins tend to dilate, causing a stagnation of blood (or blood stasis) in the dilated area. Over time, this overload of blood weakens the valves. They then let blood leak in the tissues causing swelling of the veins in the legs and feet. Weak muscle tone in the legs is another factor that may hinder blood flow in the veins.
People at risk:
Sex – 80% of varicose veins cases are from women. The problem can be due to hormonal changes associated with pregnancy, premenstrual period and menopause, which also contribute to weaken vein walls. Birth control pills and hormone replacement may also play a role in the occurrence of varicose veins in women.
Age – age plays a major role in the health of your veins. As you get older, your veins start losing their elasticity and their ability to contract. As the valves tend to diverge, their edges are no longer able to merge to prevent blood reflux, which leads eventually to varicose veins. This degeneration can begin from your thirties.
Heredity – heredity is primarily responsible for the occurrence of varicose veins. Experts from Harvard University confirm that more than 50% of people who suffer from varicose veins have inherited from their parents. That is, if you have members in your family who have varicose veins, you are at greater risk to have it.
Pregnancy – Pregnant women are at greater risk of developing varicose veins because of secretion of certain hormones during the pregnancy that tend to weaken the tone of their venous walls. In addition, the weight of the baby can affect the health of the veins. However, varicose veins which are purely related to pregnancy often resolve by themselves during the first three months following the childbirth.
Certain Professions – people who work standing for a long period of time such as nurses and servers are particularly affected by the problems of vein problems including varicose veins.
Varicose Veins Risk Factors
Combined with the risks related to age, heredity and sex, the following factors could also play a role developing varicose veins:
- Chronic constipation
- Lack of exercise
- Taking contraceptive pill
- Prolonged standing or sitting
- Exposure to heat such as sun baths, hot baths, etc.
- Repeated lifting of heavy objects, like people who practice weightlifting
- Obesity – excess weight puts an increased pressure on the venous system of your lower limbs
- Wearing tight clothes such as garters, girdles, stockings, etc.
Varicose Veins Symptoms
 If you have varicose veins, you will develop at least one of the following symptoms:
If you have varicose veins, you will develop at least one of the following symptoms:
- heavy legs
- Ankle swelling
- Restless legs syndrome
- Aching, redness, dryness, and itchiness in your affected leg (s)
- Appearance of spider veins
- Whitened or irregular scar-like patches at your ankle
- Skin discoloration (usually a brownish-blue shiny) in the skin covers the affected veins
- Tendency to abnormal bleeding during minor injuries
Complications
Although rare, severe varicosities can lead to major complications because of the poor circulation through the affected limbs.
- Pain and heaviness in your legs
- inability to walk or stand for long hours
- Skin problems such as discoloration and inflammation of the skin
- venous ulcers (especially near the ankle), which can turn into cancer
- tendency of severe bleeding from minor injuries
- necrosis at the ankle (primarily if you are overweight and a female), premature death of cells and living tissue
Diagnosis
The first step in the diagnosis of varicose veins is a physical exam. During the examination, your phlebologists will question you about the symptoms and functional signs of the disease (see Symptoms). If there is not enough evidence, your phlebologists will make a doppler ultrasonography or venography (also called phlebography) to confirm the diagnosis.
Doppler echocardiography – this medical technique consist of studying the blood flow in your vessels. It allows your health care provider to detect blood flow disturbances that may be related to phlebitis, Inflammation of a vein due to formation of blood clots; or an atherosclerotic plaque, deposit of fat and other substances that accumulate in the lining of the artery wall
Venography – also called phlebography, venography involves in injecting into your veins a contrast dye (an iodized opaque to X-rays) which allows doctor to see image of your leg veins on a fluoroscope screen. Venography can not only reveal a blood clot, but also specify the height and shape of the clot, and the seriousness with which the vein is blocked. Compared with the doppler echocardiography, venography provides more accurate images.
Varicose Veins Treatment
Treatments vary depending on the severity of the varicose veins. In moderate varicose veins, the basic treatment includes the following components: compression stockings, sclerotherapy, elevation of your legs and other preventive measures (exercising, losing weight, not wearing tight clothes, avoiding long periods of standing or sitting, etc.) aiming at avoiding more damages to your veins. In severe varicose veins, surgery can be necessary:
Compression stockings – compression stockings can be the first option your phlebologist will consider to treat your varicose veins and prevent appearance of new ones. They work by compressing the veins and prevent the accumulation of blood in them. Compression stockings can be used in painful varicose veins and those accompanied with complications such as ulcers.
However, it is important that you buy Compression stockings that are strong and fit your legs; too tight are not recommended. To wear them in all comfort, it is better to put them in the morning before getting up, in threading them in supine position. As long as possible, they should be worn all day.
Anti-inflammatory drugs – along with wearing compression stockings, your physician can prescribe you antiinflammatory medications to reduce the inflammation of your legs. Usually, they are used to relieve inflammation of superficial phlebitis.
Sclerotherapy – usually, sclerotherapy is performed without anesthesia or recovery time; it is an ideal option for minor and moderate varicose veins. Your doctor injects an irritant solution in your veins (small or medium-sized varicose veins) causing them to fade. The injection forces the blood to flow to other non-varicose veins, which render the varicose veins useless and become normal gradually. This procedure usually leaves no scars.
The results of sclerotherapy are usually satisfying; however, it may require several treatments over the same vein. In addition, sclerotherapy does prevent formation of new varicose veins.
Surgical Treatment
Ambulatory phlebectomy – During this procedure, your doctor uses a phlebectomy hook to do some tiny skin incisions (usually 1-2 millimeter) to extract small-size varioses veins on the surface of your legs.
Laser surgery – A variety of laser treatments are offered now days to treat varicose veins and spider veins. During the laser surgy, a laser fiber is inserted into the infected vein, forcing it to close in on itself. This treatment is usually used in smal varicose veins and spider veins.
Ambulatory and hemodynamic treatment of venous insufficiency (CHIVA cure) – Still under consideration, this surgery reduces the venous pressure without removing the veins. The superficial veins are tied, which forces the blood flow to pass through the deep veins. Once tied, they deflate themselves and become less visible and less painful. This intervention is aimed at treating moderate varicose vein and spider veins.
Endoscopic vein surgery – this surgical intervention is performed in serious cases where complications of the varioses veins lead to ulcers. During the procedure, your surgeon inserts a tiny video camera into your leg through a small incision so that he/she can visuliaze and treat the affected veins. Endoscopic vein surgery may require a short term hospitalization.
Vein stripping – this intervention is reserved for serious cases of varicoses veins. It consists of removing a long vein through a small incision. Depending on the severity of the problem, treatment may require hospitalization from one to five days followed by a recovery ranging from 3 to 21 days.
Varicose Veins Prevention
There is no vaccine or medications aimed at preventiinf varicoses vein; however, the following preventive measures can decrease your risk of developing the disease:
- Treat constipation before it becomes chronic
- Exercise regularly
- Avoid Prolonged standing or sitting
- Avoid Exposure to heat such as sun baths, hot baths, etc.
- Avoid repeated lifting of heavy objects
- Have a normal weight – excess weight puts an increased pressure on the venous system of your lower limbs
- Aboid wearing tight clothes such as garters, girdles, stockings, etc.



