Heart Attack
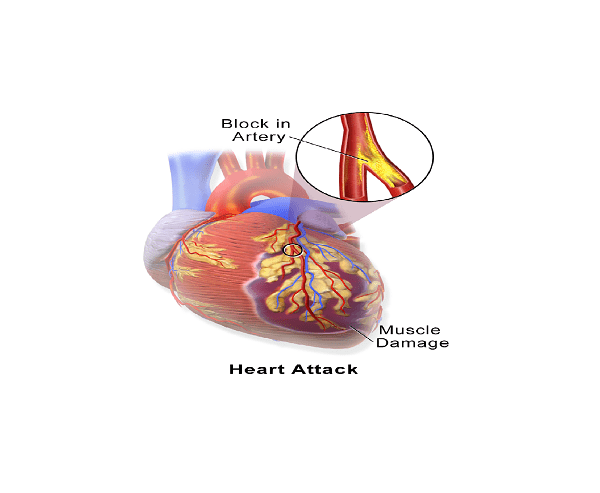
Heart attack, also called Myocardial infarction, is a sudden destruction of heart tissue due to an interruption of oxygen-rich blood supply to part of the heart muscle, the myocardium. Usually, the attack occurs when one or more coronary arteries are blocked by a clot.
The myocardium plays an important role in circulation of blood throughout the body. At each contraction, it pumps blood through the arteries to all organs of the body so that they can be irrigated and supplied with oxygen and other necessary nutrients. Unlike many other organs, the heart does not stop working; even at rest, the myocardium continues its vital job. Stopping working for a while means death.
Heart attack is not a minor issue in developed countries like the U.S. Heart disease is the number one killer in the United States. According to American Heart Association, there is an estimate of 1,260,000 new coronary attacks each year; about 37 percent of them die from it. According to the same study, nearly one of every five deaths was resulted from coronary heart disease (CHD) in 2005.
Heart Attack Causes
In general, for a heart attack to occur there must be a blockage of one or more coronary arteries (arteries supplying the heart) by a blood clot, preventing the heart to receive enough oxygen and nutrients it needs to function. If the lack of oxygen persists, premature death of cells and tissue will occur in the myocardium. Without an urgent medical intervention, this disorder will cause immediate death.
Most of the times, a heart attack is the result of atherosclerosis. Atherosclerosis results from accumulation of cholesterol, cellular debris and other fat substances in the inner lining of the arteries. With time, those substances within the wall of the arteries will transform in hard, thick cholesterol plaque, making blood flow difficult.
Although rare, a heart attack may also be due to a spasm in a coronary artery. The effect of the spasm may be minor or major. A minor spasm tends to cause a lack of oxygen in a small part of the myocardium; in this case, the pathology may pass unnoticed. A major spasm, however, can affect the whole heart or a great part of it, leading to heart attack or/and even death.
Risk Factors
Factors favoring the development of a heart attack include:
- Diabetes
- Obesity
- Physical inactivity
- Violent sports and activities
- State of psychological stress
- Sex – men are at greater risk of heart attack than are women below 55
- Age – risk of heart attack increases with age
- High homocysteine levels
- Arterial hypertension
- High blood cholesterol levels
- Family history of heart attack
- Tobacco, including passive smoking
- Certain rare coronary diseases: polyarteritis nodosa, Kawasaki disease, etc.
- Polycythemia secondary to taking erythropoietin
- Familial predisposition – if your parents have already had a heart attack, you are at higher risk.
Heart Attack Warning Signs Symptoms
 Symptoms of heart attack vary from one person to another; in addition, sex may also influence the characteristic of the symptoms. In women, the sensation of pain is similar to heartburn. The pain is often extended into the chest and may take the form of a vague discomfort.
Symptoms of heart attack vary from one person to another; in addition, sex may also influence the characteristic of the symptoms. In women, the sensation of pain is similar to heartburn. The pain is often extended into the chest and may take the form of a vague discomfort.
Most often, first indication of the heart attack warning signs is chest pain similar to a burning, squeezing or tightness. What differentiates a heart attack pain from a chest discomfort is that the chest pain occurs suddenly and is not relieved at rest. In addition, it tends to be associated with pain in left arm, neck, jaw and back. In addition, the chest pain may be associated with:
- shortness of breath
- difficulty breathing
- nausea and vomiting
- sweating
- anxiety.
Although both men and women can experience the same heart attack symptoms; women tend to experience the following:
- unreasonable fatigue
- lightheadedness or dizziness
- abdominal pain similar to heartburn
- Clammy skin – skin becomes cool, moist, and usually pale.
Complications
If you experience a sudden or prolonged chest pain, or any of these heart attack symptoms mentioned above, it is extremely important that you see your doctor right away. Heart attack warning signs should never be taken lightly; it is a matter of life or death. Most people who had a myocardial infarction (MI) tend to overlook the seriousness of the symptoms. Heart attack should not be neglected; every minute that passes increases your risk of death. If you are unable to see a doctor, call 911 right away. Even if you are lucky to survive, heart attack can lead to:
- heart failure
- heart valves damaged
- Abnormal heart rhythms.
Diagnosis
A heart attack does not always give chance for diagnosis; in fact, certain attack victims have no chance of reaching hospital. When the diagnosis is possible, a physical examination is often the first step that your cardiologist will consider. If you are conscious, he will ask you questions about your medical history and characteristics of the symptoms. After which, the cardiologist will then proceed blood tests, radiography, electrocardiography, echocardiography and angiography. These tests can help him to determine if there is heart muscle damage, and rule out other medical conditions having symptoms similar to heart attack.
Physical exam – a cardiac examination is an important part of a heart attack diagnosis. It allows your doctor to get an idea of your cardio-vascular problem. During the examination, the cardiologist will look for signs of heart failure, cardiovascular risk factors, high blood pressure, heart murmurs, abdominal aortic aneurysm, etc. Hoverer, a physical examination is not sufficient to confirm the diagnosis, other tests are needed.
Blood test – your health care provider will do a blood test to look for indication of heart attack. Increased cardiac enzymes are often a sign of myocardial cell death. The most specific enzyme of a heart attack is the troponin (I or T). Troponin tests can be associated with CK–MB or myoglobin test.
Chest X-ray – this exam allows your doctor to evaluate your lungs, heart and chest wall. A chest X-ray not only helps your cardiologist to visualize the size and shape of your heart but also to discover a heart failure and other diseases of the heart muscle.
Electrocardiogram (ECG or EKG) – an electrocardiography is a painless medical procedure which has no major contraindications. It allows your cardiologist to study and record changes in electrical activity of your heart cells. During the examination, an EKG technician attaches electrodes on different parts of your body to get a recording of variations of the rhythm of your heartbeat. The ECG can not only detect the cause of the abnormal heart rhythm but also monitor a heart attack.
Echocardiogram – An echocardiogram is the use of sound waves (ultrasound) to create picture of the heart muscle. It allows your physician to visualize and record the shape, texture and movement of the valves and the volume and function of the cardiac chambers.
Coronary catheterization (angiogram) – this exam consists of using a thin catheter along with a computerized tomography to visualize the coronary circulation and blood filled chambers of the heart. Using the CTA, your cardiologist can detect internal problems of the heart and major blood vessels like the aorta. In addition, he can see if your coronary arteries are narrowed or blocked. The CTA is also used to detect narrowing or blockage of the carotid arteries that carry blood from the heart to the brain.
Heart Attack Treatment
During and after treatment, drugs or surgical treatment, it is important to prevent or avoid all factors of cardiovascular risk: unhealthy diet, cigarette smoke, diabetes complication, obesity, physical inactivity, etc.
All form of heart attack deserves immediate medical care; you should not overlook or use “pseudo-therapies”; otherwise, you are playing with your life. While you are waiting for medical assistance, you can take an aspirin to facilitate the circulation of blood in the vessels.
In most cases of heart attack, hospitalization is required and must be made in specialized units with equipment for resuscitation and monitoring of vital signs. Usually, you will be put to strict rest, possibly on supplemental oxygen. In addition, an Ekg monitor can be established to control the activity of your heart.
Usually, two methods can be used to re-normalize the myocardial function after a heart attack: medical treatment, use of drugs to destroy the blood clot (thrombus) blocking the artery; or/and surgical treatment such as angioplasty or bypass surgery.
Medications
Medications prescribed by your cardiologist vary depending on the cause and severity of the disease. In general, your doctor will recommend you to take at least one of these drugs:
Aspirin – if case there is no contraindication, you will be recommended to take a daily dose of aspirin. The most common dose is between 80 and 81 mg once daily for a long period of time or for life. Along with a healthy diet and exercise, aspirin can reduce the risk of a new occlusion of your coronary arteries, thus, preventing another heart attack.
Beta-blockers: beta blockers are used effectively in all types of heart attack, regardless of the severity and extent of the disease; however, they seem more beneficial for patients who have a serious heart attack. Along with a healthy diet, beta-blockers can help reduce adrenergic blood pressure on your heart. In addition, these drugs reduce the risk of another heart attack or progression of heart failure in patients having a previous heart attack. The most commonly used in the treatment of heart attack include: metoprolol (Lopressor, Toprol XL), atenolol (Tenormin) and bisoprolol (Zebeta).
Angiotensin–converting enzyme (ACE) inhibitors – As beta-blockers do, this class of medications help control blood pressure and reduce cardiac remodeling, changes in the size and function of the heart which can lead to heart failure. Your cardiologist will recommend you to take ACE inhibitors even if your blood pressure is normal. If you develop intolerance, you will be prescribed satins. Usually, you will be asked to take ramipril (Altace) or enalapril (Vasotec) in the class of ACE inhibitors.
Statins – satins are used to lower levels of high blood cholesterol and reduce the risk of a new heart attack. Among the satins, the most used in the treatment of heart attack are atorvastatin (Lipitor), simvastatin (Zocor) and pravastatin (Pravachol). As beta-blockers, these medications must be taken for a long term.
Clopidogrel – This antiplatelet drug, along with aspirin, is used to reduce the risk of thrombosis, presence of blood clot in your blood vessel. In most cases, your cardiologist will prescribe this medication if you have been treated with stent implantation. You may be recommended to take clopidogrel in combination with aspirin for at least 1 year.
Surgery
Coronary angioplasty – After a severe heart attack which does not respond well to medications, angioplasty or coronary bypass surgery can be necessary. In this case, a cardiovascular surgeon will install, temporarily, a balloon catheter within the aorta that acts as an auxiliary pump which performs some of the works of the heart. Although rare, angioplasty can lead to complications no matter how good the surgeon is. Research on angioplasty is ongoing to make it safer and more effective in the fight against coronary disease.
Coronary Artery Bypass Surgery – the coronary arteries are small blood vessels (2 to 3 mm in diameter) arising at the origin of the aorta above the aortic valve. Their main job is to supply the heart with oxygen-rich blood. These arteries, however, may be narrowed or blocked by deposits of fat, which prevents the heart to find sufficient nutrients and oxygen needed to function properly. A coronary artery bypass surgery is performed to bypass the blocked artery by a blood vessel graft to restore normal blood flow to the heart. This intervention is indicated for the prevention of sudden death, mainly in patients with heart disease with mechanical malfunction of the left ventricle.
Heart Attack Prevention
It is important to prevent any possible risk factors leading to heart attack; although it is not always easy for some people, practicing the following preventive measures can help you prevent not only cardiovascular diseases but also a variety of other ailments including many types of cancer.
- Do not smoke
- Avoid stress
- Exercise regularly (get your doctor approval if you have heart disease)
- Maintain a healthy weight
- Control your blood pressure
- Avoid heavy alcohol consumption
- Maintain normal blood cholesterol levels.
Adopt a heart-healthy diet – eating plenty of fruits and vegetables; they are rich in nutrients that can help the heart and blood vessels to accomplish their function. Being rich in antioxidants and fiber, fruits and vegetables help prevent oxidation of cholesterol, which contributes in the formation of blood clot. Regular eating of a diet consisting mainly of fruits and vegetables can prevent the development of cardiovascular disease, leading causes of death in developed countries.
1 – Hardoon SL, Whincup PH, Lennon LT et Als. How much of the recent decline in the incidence of myocardial infarction in british men can be explained by changes in cardiovascular risk factors?: evidence from a prospective population-based study
2 – American Heart Association: Final 2005 statistics for the United States show that coronary heart disease (CHD) is the single leading cause of death in America. CHD causes heart attack and angina.
3 – Antiplatelet Trialists’ Collaboration. Collaborative overview of randomized trials of antiplatelet therapy. I : prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Br Med J 1994; 308: 81-106.
4 – Coronary Drug Project Research Group.Aspirin in coronary heart disease. J Chron Dis 1976; 29:625-42.
5 – Aspirin Myocardial Infarction Study Research Group.A randomized, controlled trial of aspirin in persons recovered from myocardial infarction. JAMA 1980; 243: 661-9.
6 – de Araujo Goncalves P, Ferreira J, Aguiar C, Seabra-Gomes R, TIMI, PURSUIT, and GRACE risk scores: sustained prognostic value and interaction with revascularization in NSTE-ACS , Eur Heart J 2005;26:865-872
7 – Chen ZM, Jiang LX, Chen YP et als. Addition of clopidogrel to aspirin in 45,852 patients with acute myocardial infarction: randomised placebo-controlled trial, Lancet, 2005;366:1607-1621
8 – White HD, Chew DP, [372:570-584 Acute myocardial infarction], Lancet, 2008;372:570-584
9 – Wijeysundera HC, Vijayaraghavan R, Nallamothu BK et als. Rescue angioplasty or repeat fibrinolysis after failed fibrinolytic therapy for ST-segment myocardial infarction: a meta-analysis of randomized trials, J Am Coll Cardiol, 2007;49:422-430
10 – Keeley EC, Boura JA, Grines CL, Comparison of primary and facilitated percutaneous coronary interventions for ST-elevation myocardial infarction: quantitative review of randomised trials , Lancet, 2006;367:579-588
11 – Collet JP, Montalescot G, Le May M et als. Percutaneous coronary intervention after fibrinolysis: a multiple meta-analyses approach according to the type of strategy, J Am Coll Cardiol, 2006;48:1326-1335
12 – Hochman JS, Lamas GA, Buller CE et als. Coronary intervention for persistent occlusion after myocardial infarction, N Engl J Med, 2006;355:2395-2407.
13 – Moran, AE; Forouzanfar, MH; Roth, GA; Mensah, GA; Ezzati, M; Flaxman, A; Murray, CJ; Naghavi, M (8 April 2014). “The global burden of ischemic heart disease in 1990 and 2010: the Global Burden of Disease 2010 study.”. Circulation 129 (14): 1493–501. doi:10.1161/circulationaha.113.004046. PMID 24573351.
14 – National Heart, Lung and Blood Institute. Heart Attack Warning Signs. Retrieved November 22, 2006.
15 – Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, Fox K, Huber K, Kastrati A, Rosengren A, Steg PG, Tubaro M, Verheugt F, Weidinger F, Weis M (December 2008). “Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: the Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology”. Eur. Heart J. 29 (23): 2909–45. doi:10.1093/eurheartj/ehn416. PMID 19004841
16 – Mendis, Shanthi; Puska,, Pekka; Norrving, Bo (2011). Global atlas on cardiovascular disease prevention and control (PDF) (1st ed.). Geneva: World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization. pp. 3–18. ISBN 9789241564373.
17 – “What Causes a Heart Attack?”. http://www.nhlbi.nih.gov. December 17, 2013. Retrieved 24 February 2015.
18 – Devlin, RJ; Henry, JA (2008). “Clinical review: Major consequences of illicit drug consumption.”. Critical care (London, England) 12 (1): 202. doi:10.1186/cc6166. PMC 2374627. PMID 18279535.
19 – “How Is a Heart Attack Diagnosed?”. http://www.nhlbi.nih.gov/. December 17, 2013. Retrieved 24 February 2015.
20 – McSweeney JC, Cody M, O’Sullivan P, Elberson K, Moser DK, Garvin BJ (2003). “Women’s early warning symptoms of acute myocardial infarction”. Circulation 108 (21): 2619–23. doi:10.1161/01.CIR.0000097116.29625.7C. PMID 14597589.
22- Davis TM, Fortun P, Mulder J, Davis WA, Bruce DG (2004). “Silent myocardial infarction and its prognosis in a community-based cohort of Type 2 diabetic patients: the Fremantle Diabetes Study”. Diabetologia 47 (3): 395–9. doi:10.1007/s00125-004-1344-4. PMID 14963648.
23 – Rubin, Emanuel; Gorstein, Fred; Rubin, Raphael; Schwarting, Roland; Strayer, David (2001). Rubin’s Pathology — Clinicopathological Foundations of Medicine. Maryland: Lippincott Williams & Wilkins. p. 549. ISBN 0-7817-4733-3.
24 – Acute Coronary Syndrome. American Heart Association. Retrieved November 25, 2006. Archived September 25, 2006, at the Wayback Machine.
25 – Mozaffarian D, Micha R, Wallace S (2010). Katan, Martijn B, ed. “Effects on Coronary Heart Disease of Increasing Polyunsaturated Fat in Place of Saturated Fat: A Systematic Review and Meta-Analysis of Randomized Controlled Trials”. PLoS Med. 7 (3): e1000252. doi:10.1371/journal.pmed.1000252. PMC 2843598. PMID 20351774.
26 – McPherson K, et al. (June 2010). “Prevention of cardiovascular disease – NICE public health guidance 25”. London: National Institute for Health and Care Excellence.
27 – Antithrombotic Trialists’ (ATT), Collaboration; Baigent, C; Blackwell, L; Collins, R; Emberson, J; Godwin, J; Peto, R; Buring, J; Hennekens, C; Kearney, P; Meade, T; Patrono, C; Roncaglioni, MC; Zanchetti, A (30 May 2009). “Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials.”. Lancet 373 (9678): 1849–60. doi:10.1016/S0140-6736(09)60503-1. PMC 2715005. PMID 19482214.
28 – Sutcliffe, P; Connock, M; Gurung, T; Freeman, K; Johnson, S; Kandala, NB; Grove, A; Gurung, B; Morrow, S; Clarke, A (September 2013). “Aspirin for prophylactic use in the primary prevention of cardiovascular disease and cancer: a systematic review and overview of reviews.”. Health technology assessment (Winchester, England) 17 (43): 1–253. doi:10.3310/hta17430. PMID 24074752.
29 – Matthys, F; De Backer, T; De Backer, G; Stichele, RV (March 2014). “Review of guidelines on primary prevention of cardiovascular disease with aspirin: how much evidence is needed to turn a tanker?”. European journal of preventive cardiology 21 (3): 354–65. doi:10.1177/2047487312472077. PMID 23610452.
30 – Hodis, Howard (July 2014). “Hormone replacement therapy and the association with coronary heart disease and overall mortality: Clinical application of the timing hypothesis”. The Journal of Steroid Biochemistry and Molecular Biology 142: 68–75. doi:10.1016/j.jsbmb.2013.06.011. PMID 23851166